Restoration of the Edentulous Maxilla Using Extrasinus Zygomatic Implants Combined with Anterior Conventional Implants: A Retrospective Study
Reginaldo Mário Migliorança, PhD, DDS, MSc1 /Abílio Coppedê, DDS, MSc2 /Renata C. L. Dias Rezende, DDS2 /Thiago de Mayo, DDS2
Purpose: To report on the clinical outcome of 150 extrasinus zygomatic implants placed lateral to the maxillary sinus and combined with conventional implants in the anterior maxilla for the implant-supported rehabilitation of the edentulous maxilla. Materials and Methods: All patients included in this study presented with completely or partially edentulous maxillae with any remaining teeth indicated for extraction. Indications for extractions in partially edentulous patients included longitudinal fractures, periodontal disease, endodontic failure, perforated roots, and prosthetic convenience. All patients showed severe resorption of the posterior maxilla. Each patient was treated with at least four implants, with a minimum of one zygomatic implant. No bone grafting was performed. The zygomatic implants were placed outside the sinus, lateral to the maxillary sinus.
The patients were followed with standardized clinical and radiographic examinations. Results: Seventy-five patients with severely atrophic maxillae (mean age, 52 years) were treated between 2003 and 2006. In all, 436 implants (150 zygomatic implants and 286 conventional implants) were placed. Two conventional implants failed during the study period, and two zygomatic implants were removed. All the prostheses were successful. No patients presented sinusitis. No loosened or fractured screws on any implants were recorded. Conclusion: Extrasinus zygomatic implants, when combined with conventional implants in the anterior maxilla, represent a predictable treatment option for the atrophic edentulous maxilla. Further studies are necessary to evaluate the long-term prognosis of these implants. Int J Oral Maxillofac Implants 2011;26:665–672.
Key words: atrophic maxilla, dental implants, maxillary sinus, zygomatic implants
The treatment of patients with severe maxillary atrophy is a considerable challenge in oral rehabilitation.1,2 Tooth loss leads to continued, cumulative, and irreversible bone loss in the maxilla and mandible. 3–5 The absence of the teeth and the alveolar ridges causes functional and esthetic problems, such as loss of chewing ability 6 and loss of labial support.7 The lack of labial support leads to facial sulcus enhancement, which results in premature aging.7 In addition to these physical problems, edentulous patients are also affected psychologically. 8 Immediately after tooth extraction, the residual alveolar ridge usually has sufficient height and width to allow satisfactory dentures to be constructed. 9–13 However, as a result of bone loss caused by the continued use of conventional dentures, some prostheses may present functional limitations owing to a lack of suitable retention, support, and stability.9–13 The shortage of dense bone and the presence of the sinus in the maxilla in association with a resorbed alveolar ridge make implant placement difficult.14–19 Sinus lift procedures and onlay bone grafting have been described as methods to restore the architecture of the atrophic maxilla and allow implant placement.14–19 However, bone grafting usually requires two surgical sites when host bone is used, which can make the postsurgical period uncomfortable.
Also, the use of removable dentures during the healing period may be contraindicated. Finally, the treatment may demand considerable time until definitive prostheses are delivered. An alternative to major reconstructive procedures is the zygomatic implant. At first, these implants were used to treat patients with cleft palate or after maxil-lectomy. Currently, zygomatic implants are also used in patients with atrophic maxillae. The original placement technique recommends that these implants should be placed through the maxillary sinus andbanchored apically in the zygomatic bone. 20 The extrasinus placement of the zygomatic implant proposed in the present study is intended to simplify surgical procedures and to improve prosthetic outcomes.
The aim of this study was to evaluate the outcome of the restoration of the atrophic edentulous maxilla with extrasinus zygomatic implants in combination with anterior conventional implants to retain full-arch screw-retained prostheses.
Materials and Methods
Presurgical evaluation
Subjects presented for treatment in a private office in Campinas, São Paulo, Brazil. All patients included in this study presented with completely or partially edentulous maxillae; any remaining teeth were indicated for extraction. The indications for extractions in partially dentate patients included longitudinal fractures, periodontal disease, endodontic failure, perforated roots, and prosthetic convenience. The inclusion criteria were: need for rehabilitation of the maxilla with a complete fixed implant-supported prosthesis, ability and willingness of the patient to follow the study protocol, and a good state of general health and oral hygiene. Maxillary bone volume was assessed by means of radiographic measurements.
Patients needed to have atrophy of the maxillary bone for inclusion in this study of division C or D, as suggested by Misch 21; a bone height of at least 10 mm in the anterior maxilla to allow the placement of two anterior implants with a minimum length of 10 mm; and posterior maxillary bone height immediately distal to the canine pillar between 1 and 3 mm (ie, insufficient to allow the placement of conventional implants).
Patients who did not present with these bone dimensions were excluded. Other exclusion criteria were general and local health conditions that prevented the use of general anesthesia and/or intraoral surgery; general conditions that could lead to problems with osseointegration, such as the use of bisphosphonates for osteoporosis treatment; parafunctional habits, such as bruxism; and poor oral hygiene. Smoking was not utilized as an exclusion criterion.
No bone grafting procedures were performed. All possible treatment options were offered to the patients. Patients who enrolled in the study authorized the procedure by signing a consent form according to the Helsinki Declaration (1975, revised in 2000). Diagnosis and treatment planning included study models articulated in a semiadjustable articulator, a diagnostic waxup, clinical photographs, and panoramic and Waters view radiographs to identify the anatomical structures and detect any pathologies. surgical Protocol Patients were medicated with 2 g of cephalexin intra-venously before the surgical procedure.
For patients who were allergic to cephalosporins, 500 mg of ciprofloxacin was administered intravenously. Immediately before surgery, patients rinsed with 2% chlorhexidine mouthwash for 30 seconds. General anesthesia was used for all surgical procedures, and pulse, blood pressure, and pulse oximetry were monitored by an anesthesiologist. A local anesthetic of 2% mepivacaine with 1:100,000 epinephrine was infiltrated supracrestally to limit bleeding. A supracrestal incision joining both tuberosities was made, along with two vertical releasing incisions in the zygomatic pillar region.
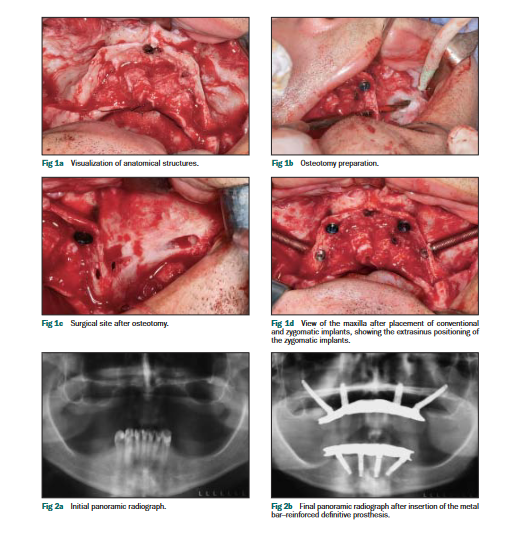
A mucoperiosteal flap was reflected, allowing the anatomical structures to be visualized. Osteotomies for the placement of the conventional implants (Replace Select Tapered, Nobel Biocare) were performed according to the instructions of the manufacturer. The insertion torque was adjusted with drilling equipment at an initial insertion torque of 35 cm. If the handpiece “stalled,” the implant was inserted manually with a torque wrench until it was completely seated.
The zygomatic implants (Brånemark System, Nobel Biocare) were placed outside the sinus, contacting the outer aspect of the lateral wall of the maxillary sinus, as distal as the anatomy of the patient allowed, preferably in the second premolar or first molar region. No maxillary antrostomy was necessary. The osteotomies for the zygomatic implants began with a spherical drill, which penetrated the residual ridge near to the top of the crest, from palatal to buccal, transfixed it, and emerged in the buccal aspect of the ridge, external to the maxillary sinus.
The drilling continued toward the zygomatic bone along the outer aspect of the lateral wall of the maxillary sinus until it reached the zygomatic bone in its lateral portion. With the same drill, the zygomatic bone was perforated until the outer cancellous layer of the bone was surpassed. The depth indicator was then used to determine the length of the zygomatic implant, which was defined as 2 mm less than the obtained measurement. The osteotomy was progressively widened using these drills in sequence: twist drill 2.9 mm, pilot drill 2.9/3.5 mm, twist drill 3.5 mm.
The implants were placed with an initial insertion torque of 40 Ncm, after which insertion was completed manually. The platforms of the zygomatic implants emerged over or close to the top of the crest of the residual alveolar ridge. Straight multiunit abutments (Nobel Biocare) were tightened to the implants with 32 Ncm of torque. The surgical wounds were sutured with 4-0 Vicryl after the abutments were placed. The surgical procedure and presurgical and postsurgical panoramic radiographs are illustrated in Figs 1 and 2.
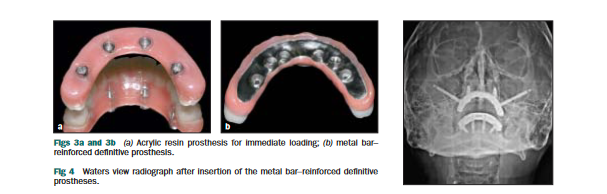
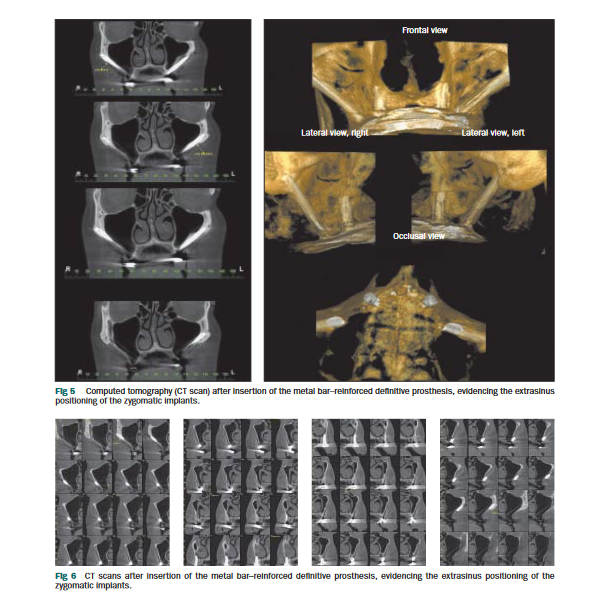
igliorança et al 668 Volume 26, Number 3, 2011 Patients were asked to rinse with 2% chlorhexidine mouthwash three times daily after surgery. Amoxicillin (875 mg) was prescribed two times a day for 7 days. For penicillin-allergic subjects, 500 mg ciprofloxacin twice a day for 7 days was prescribed. Prosthetic Protocol The implant-supported screw-retained prostheses were fabricated in two different ways according to loading time (immediate or delayed). The acrylic resin prostheses for immediate loading were planned postsurgically for all patients in whom the implants showed adequate primary stability (ie, over 40 Ncm 22 of insertion torque). Impressions of the implants and the residual ridge were made immediately after surgery with open-tray transfers and splinted with a lowshrinkage modeling resin (Pattern Resin, GC America).
After the resin had polymerized completely, the segments between transfers were sectioned with a surgical scissor; these sectioned portions were then united with a small amount of the same resin to minimize polymerization shrinkage. Impressions were made with plastic trays perforated in the sites of the transfers. Only the putty soft additio silicone material (Elite Putty Soft Normal, Zhermack) was used; no lightbody material was used in the impressions to avoid penetration of this material into the surgical wound, which could cause local irritation and further complications. Working casts were obtained, and implant-screwed wax rims were fabricated in these models.
All maxillomandibular relations were recorded in these screwed wax rims on the day after surgery. Esthetic and functional try-ins of the artificial teeth were performed, and a soon as they were approved, the prostheses were finalized. The all–acrylic resin provisional prostheses were attached to the implants with titanium cylinders embedded in the heat-polymerized acrylic resin 24 hours after surgery. Six months after placement, the provisional prostheses were replaced by definitive metal bar–reinforced prostheses.
For patients with one or more implants without adequate primary stability, the prostheses for delayed loading were constructed 6 months after surgery; they were reinforced with metal bars. Throughout this period, patients wore conventional removable prostheses relined with soft silicon liners (Ufi Gel, VOCO). The two types of prostheses used in this study are shown in Fig 3.
Follow-up
Patients were followed for a minimum of 12 months after loading. Each implant was classified as surviving if it fulfilled its supportive function and was stable when tested individually. The success criteria utilized in this study were: absence of pain, stability of the implants, normal probing depths, lack of excessive bone resorption, absence of excessive bleeding, and radiographic success, as suggested by Misch. 23 Implant clinical conditions were assessed at all follow-up appointments (every 3 months during the first year and semiannually thereafter); patients were examined by means of periodontal probing, radiographs, and intraoral and extraoral photographs.
For biofilm control, all patients were instructed to use interdental brushes, dental floss, and an oral hygiene system based on high-pressure water spray twice a day. Pan- oramic (Fig 2) and Waters view (Fig 4) radiographs were taken before and after surgery, after prosthesis placement, and at semiannual appointments. After the second follow-up visit, screw-retained prostheses were removed at every appointment for professional intraoral hygiene and laboratory polishing of the prostheses.
Upon reinsertion, new screws were used. The examination at the follow-up appointments included assessment of oral hygiene, soft tissue health (peri-implant pockets, pain, exudate), radiographic aspects of the bone-implant interface, implant and prosthesis stability, screw loosening, and other mechanical complications. Computed tomographic (CT) scans were obtained after the definitive prosthesewere placed (Figs 5 and 6).
Results
Seventy-five patients (27 men and 48 women), withages ranging from 32 to 81 years (mean: 52 years), were included in this study, and clinical data were collected
from 2003 to 2006. Each patient was treated with a minimum of four implants, which included at least one zygomatic implant. Altogether, 436 implants (150 zygomatic implants and 286 conventional implants) were placed. Sixty patients presented with edentulous maxillae and 15 were partially edentulous with their remaining teeth indicated for extraction. Fifty-eight patients were smokers (77.3%). Eight subjects had been previously treated with implants, and none had received bone grafting prior to this study.
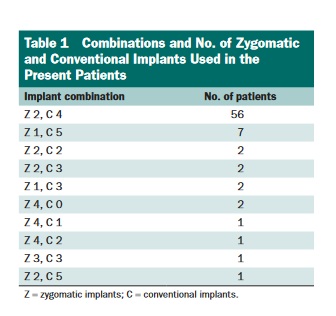
All 75 patients were treated with a combination of conventional and zygomatic implants supporting fixed full-arch screw-retained dental prostheses. The combinations of zygomatic and conventional implants used in the patients are listed in Table 1. Twenty-seven patients had their implants immediately loaded with screw-retained all–acrylic resin fixed prostheses 24 hours after the surgery. The other 48 patients had their submerged implants uncovered and definitive prostheses delivered approximately 6 months after surgery. All patients received and maintained a fixed full-arch denture during the study.
All 75 screw-retained fixed complete dentures were removed after the second follow-up appointment, and the implants were classified as successful, surviving, or failed. Two conventional implants (0.7%) failed during the study period. Two zygomatic implants (1.3%) failed and were removed. The success rate observed for the conventional implants was 99.3%, anfor the zygomatic implants was 98.7%. None of thfailed implants were replaced at this point. None of the surviving conventional implants showed signs of peri-implantitis or soft tissue dehiscences. Two surviving zygomatic implants showed a soft tissue dehiscence in the cervical portion of the implant that reached approximately the level of the second thread of the implant; no sign of irritation or inflammation was observed around these two implants.
No other soft tissue complications were observed in the other surviving zygomatic implants. The survival rate of the all-acrylic and metal-reinforced prostheses was 100%. No loosening or fractures of the zygomatic and conventional implant screws or of the prosthetic screws were recorded. No fractures of the prostheses were recorded. Patients with failed implants continued to use all-acrylic prostheses, which were modified to adapt to the new implants placed; thus, these prostheses were not lost. No patient using a metal bar–reinforced prosthesis presented with implant failures.
DisCussion
Rehabilitation of atrophic maxillae using zygomatic implants may be performed as an alternative to preimplantation bone grafting procedures. Success rates of about 85% have been reported for implants in maxillae reconstructed with iliac crest bone 22,24,25; this climbs to 90% for implants placed in elevated sinuses. 26,27 The typical success rate for zygomatic implant rehabilitation found in the literature is about 97%. 28–33 The success rate obtained in the present study (98.7%) is similar to that seen in the literature, showing that the extrasinus technique can be a feasible alternative for rehabilitating the atrophic edentulous maxilla.
Extremely resorbed residual alveolar ridges and pneumatized maxillary sinuses make the maxilla a challenging site for conventional implant placement. Under these conditions, zygomatic implants may be an important option for rehabilitating atrophic maxillae without bone grafts. 28–33 The extrasinus technique for placement of zygomatic implants used in this retrospective study is simpler than the original technique proposed by Brånemark and coworkers 20,33 and the slot technique proposed by Stella and Warner. 34 The extrasinus approach eliminates the need for maxillary antrostomy, sinus elevation, or the creation of a slot. It also results in the emergence of the zygomati implant next to or on the top of the alveolar ridge crest, improving prosthesis design and biomechanics.
In contrast, the palatal implant emergence that is typically seen with intrasinus techniques increases the risk of occlusal overload and makes oral hygiene more difficult. The potential problems related to leaving a considerable portion of the implant exposed to the overlying soft tissue include dehiscence, irritation, and inflammation. The only type of soft tissue complication observed in this study was a dehiscence in the cervical portion of two zygomatic implants; neither was associated with irritation or inflammation. The absence of inflammatory problems in these dehiscence areas, as well as in all other implants surveyed here, is directly related to the strict control protocol with periodic professional hygiene in which every patient enrolled in this study was included. No other soft tissue problems were observed with the remaining conventional or zygomatic implants.
The extrasinus technique improves the prosthetic positioning of the implant platform; eliminates the presence of the implant in the interior of the maxillary sinus, thereby avoiding the risk of sinus problems; reduces surgical time; and improves surgical visualization. The effectiveness of the zygomatic implant in the rehabilitation of the atrophic edentulous maxilla is dependent on a rigid connection between implants, which must be provided by a one-piece rigid prosthesis that includes all the implants. 20 In this study, the provisional prostheses were fabricated in acrylic resin for immediate loading, and metal bar–reinforced prostheses were used for delayed loading or as definitive prostheses for the immediate loading cases (Fig 3).
The two types of prostheses showed similar success rates. No complications were reported regarding the use of the provisional acrylic resin prostheses during the osseointegration period. In patients with implant failures, the same all–acrylic resin prostheses continued to be used; they were simply modified to accommodate the prosthetic components of newly placed implants.
ACKnowledgMents
We are extremely grateful to the laboratory technician Ricardo T. Nagahisa and his staff, who performed all the prosthetic work in this study.
ReFerenCes
1. Moore DJ, Hansen PA. A descriptive 18-year retrospective review of subperiosteal implants for patients with severely atrophied edentulous mandibles. J Prosthet Dent 2004;92: 145–150.
2. Cheng AC, Kwok-Seng L, Wee AG, Tee-Khin N. Prosthodontic management of edentulous patient with limited oral access using implant-supported prostheses: A clinical report. J Prosthet Dent 2006;96:1–6
3. Ozkan Y, Ozcan M, Akoglu B, Ucankale M, Kulak-Ozkan Y. Three-year treatment outcomes with three brands of implants placed in the posterior maxilla and mandible of partially edentulous patients. J Prosthet Dent 2007;97:78–84.
4. Bischof M, Nedir R, Abi Najm S, Szmukler-Moncler S, Samson J. A five-year life-table analysis on wide neck ITI implants with prosthetic evaluation and radiographic analysis: Results from a private practice. Clin Oral Implants Res 2006;17:512–520.
5. Fischer K, Stenberg T. Three-year data from a randomized, ontrolled study of early loading of single-stage dental implants supporting maxillary full-arch prostheses. Int J Oral Maxillofac Implants 2006;21:245–252.
6. Takata Y, Ansai T, Awano S, et al. Chewing ability and quality of life in an 80-year-old population. J Oral Rehabil 2006;33: 330–334.
7. Kamashita Y, Kamada Y, Kawahata N, Nagaoka E. Influence of lip support on the soft-tissue profile of complete denture wearers. J Oral Rehabil 2006;33:102–109.
8. Fiske J, Davis DM, Frances C, Gelbier S. The emotional effects of tooth loss in edentulous people. Br Dent J 1998;184:90–93.
9. Carlsson GE. Clinical morbidity and sequelae of treatment with complete dentures. J Prosthet Dent 1997;79:17–23.
10. Bergman B, Carlsson GE. Clinical long-term study of complete denture wearers. J Prosthet Dent 1985;53:56–61.
11. Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: A mixed-longitudinal study covering 25 years. J Prosthet Dent 1972;27:120– 32.
12. Jackson RA, Ralph WJ. Continuing changes in the contour of the maxillary residual alveolar ridge. J Oral Rehabil 1980;7: 245–248.
13. Kelsey CC. Alveolar bone resorption under complete dentures. J Prosthet Dent 1971;25:152–161.
14. Aboul-Hosn S, Monner A, Juarez I, et al. Tibial bone harvesting technique for filling maxillary bone gaps in implantology. Rev Stomatol Chir Maxillofac 2006;107:93–97.
15. Hallman M, Mordenfeld A, Strandkvist T. A retrospective 5-year follow-up study of two different titanium implant surfaces used after interpositional bone grafting for reconstruction of the atrophic edentulous maxilla. Clin Implant Dent Relat Res 2005;7:121–126.
16. Baccar MN, Laure B, Chabut A, Bonin B, Romieux G, Goga D. Stability of grafts and implants after bone grafting of the maxillary sinus. Retrospective analysis of 44 patients. Rev Stomatol Chir Maxillofac 2005;106:153–156.
17. Iturriaga MT, Ruiz CC. Maxillary sinus reconstruction with calvarium bone grafts and endosseous implants. J Oral Maxillofac Surg 2004;62:344–347.
18. Smiler DG, Johnson PW, Lozada JL, et al. Sinus lift grafts and endosseous implants. Treatment of the atrophic posterior maxilla. Dent Clin North Am 1992;36:151–186.
19. Wood RM, Moore DL. Grafting for the maxillary sinus with intraoral harvested autogenous bone prior to implant placement. Int J Oral Maxillofac Implants 1988;3:209–214.
20. Brånemark PI. Zygoma Fixture: Clinical Procedures. Göteborg, Sweden: Nobel Biocare, 2000.
21. Misch CE. Divisions of available bone in implant dentistry. Int J Oral Implantol 1990;7:9–17.
22. Duskova M, Kot’ova M, Urban F, et al. Reconstruction of maxilla alveolus for application of dental implant in patients with cleft defect. Acta Chir Plast 2004;46:115–121.
23. Misch CE. Implant success or failure: Clinical assessment in implant dentistry. In: Misch CE. Contemporary Implant Dentistry. St Louis: Mosby, 1993:33–66.
24. van der Meij EH, Blankestijn J, Berns RM, et al. The combined use of two endosteal implants and iliac crest onlay grafts in the severely atrophic mandible by a modified surgical approach. Int J Oral Maxillofac Surg 2005;34:152–157.
25. Nystrom E, Ahlqvist J, Legrell PE, Kahnberg KE. Bone graft remodelling and implant success rate in the treatment of the severely resorbed maxilla: A 5-year longitudinal study. Int J Oral Maxillofac Surg 2002;31:158–164.
26. Hatano N, Shimizu Y, Ooya K. A clinical long-term radiographic evaluation of graft height changes after maxillary sinus floor augmentation with a 2:1 autogenous bone/xenograft mixture and simultaneous placement of dental implants. Clin Oral Implants Res 2004;15:339–345.
27. Cavicchia F, Bravi F, Petrelli G. Localized augmentation of the maxillary sinus floor through a coronal approach for the placement of implants. Int J Periodontics Restorative Dent 2001;21:475–485.
28. Hirsch J-M, Henry P, Andreasson L, et al. A clinical evaluation of the zygoma fixture. One-year follow-up at 16 clinics. J Oral Maxillofac Surg 2004;9(suppl):22–29.
29. Aparicio C, Ouazzani W, Garcia R, Arevalo X, Muela R, Fortes V. A prospective clinical study on titanium implants in the zygomatic arch for prosthetic rehabilitation of the atrophic edentulous maxilla with a follow-up of 6 monhs to 5 years. Clin Implant Dent Relat Res 2006;8:114–122.
30. Bedrossian E, Rangert B, Stumpel L, Indresano T. Immediate function with the zygomatic implant: A graftless solution for the patient with mild to advanced atrophy of the maxilla. Int J Oral Maxillofac Implants 2006;21:937–942.
31. Ahlgren F, Storksen K, Tornes K. A study of 25 zygomatic dental Implants with 11 to 49 months’ follow-up after loading. Int J Oral Maxillofac Implants 2006;21:421–425.
32. Nakai H, Okazaki Y, Ueda M. Clinical application of zygomatic implants for rehabilitation of the severely resorbed maxilla: A clinical report. Int J Oral Maxillofac Implants 2003;18:566–570.
33. Brånemark PI, Grondahl K, Ohrnell LO, et al. Zygoma fixture in the management of advanced atrophy of the maxilla: Technique and long-term results. Scand J Plast Reconstr Surg Hand Surg 2004;38:70–85.
34. Stella JP, Warner MR. Sinus slot technique for simplification and improved orientation of zygomaticus dental implants: A technical note. Int J Oral Maxillofac Implants 2000;15:889–893.
