Effect of repeated torque/mechanical loading cycles on two different abutment types in implants with internal tapered connections: an in vitro study
Key words: dental implants, internal tapered connection, loosening torque, prosthesis and implants, tightening torque
Abstract
Objectives: Internal tapered connections were developed to improve biomechanical properties and to reduce mechanical problems found in other implant connection systems. The purpose of this study was to evaluate the effects of mechanical loading and repeated insertion/removal cycles on the torque loss of abutments with internal tapered connections. Material and methods: Sixty-eight conical implants and 68 abutments of two types were used.
They were divided into four groups: groups 1 and 3 received solid abutments, and groups 2 and 4 received two-piece abutments. In groups 1 and 2, abutments were simply installed and uninstalled; torque-in and torque-out values were measured. In groups 3 and 4, abutments were installed, mechanically loaded and uninstalled; torque-in and torque-out values were measured. Under mechanical loading, two-piece abutments were frictionally locked into the implant; thus, data of group 4 were catalogued under two subgroups (4a: torque-out value necessary to loosen the fixation screw; 4b: torque-out value necessary to remove the abutment from the implant). Ten insertion/removal cycles were performed for every implant/abutment assembly.
Data were analyzed with a mixed linear model (P0.05). Results: Torque loss was higher in groups 4a and 2 (over 30% loss), followed by group 1 (10.5% loss), group 3 (5.4% loss) and group 4b (39% torque gain). All the results were significantly different. As the number of insertion/removal cycles increased, removal torques tended to be lower. It was concluded that mechanical loading increased removal torque of loaded abutments in comparison with unloaded abutments, and removal torque values tended to decrease as the number of insertion/removal cycles increased.
Mechanical complications such as screw loosening, screw fractures, implant frac-tures or component fractures still play an important role in implant therapy (Good-acre et al. 1999; chwarz 2000; Cho et al.
2004). Screw loosening seems to be the most common mechanical complication in implant-supported prostheses, especially in single-tooth restorations (Goodacre et al. 1999; chwarz 2000). The external hex connection systems are more prone to screw loosening, due to their mechanical properties under dynamic loading (Henry et al. 1996; Boggan et al. 1999; Aboyoussef et al. 2000; Cho et al. 2004; Khraisat et al. 2004; Akour et al. 2005).
Internal connection systems were con-ceived to minimize such occurrences. In-ternal hex connections showed significant biomechanical advantages over the external hex onnections, such as: a better force distribution under mechanical loading; higher stability, because of a wider area of connection; and higher resistance to lateral loads, because of the lower center of rota-tion (Maeda et al. 2006). However, internal hex connections presented some disadvan-tages, such as thinner lateral fixture walls at the connecting part, difficulty in adjust-ing divergences in angles between fixtures (Maeda et al. 2006) and more rotational freedom (Carrilho et al. 2005).
Internal tapered connections were devel-oped to improve the biomechanical proper-ties of implant/abutment assemblies, and to reduce the incidence of mechanical problems found in other implant connection systems (Bozkaya & Mu ̈ftu ̈ 2003, 2005).
Comparative studies have shown that im-plants with internal tapered connections have superior dynamic and static strength (Norton 1997; Merz et al. 2000; Khraisat et al. 2002), and superior resistance to screw loosening (Kitagawa et al. 2005), whencompared with external hex implants.
A laboratory study that applied cyclic dynamic axial and lateral loads has shown high fatigue resistance and high removal torque values for implants with internal tapered connections (C ̧ ehreli et al. 2004). A 2-year retrospective study showed few mechanical complications with the clinical use of 80 internal tapered connection implants (Mangano & Bartolucci 2001).
Occlusal forces seem to play an impor-tant role in screw loosening of implants with hex connections, where the preload is the only force that resists functional occlu-sal forces in order to keep the abutment from separating from the implant. If the preload is exceeded by the occlusal force, the screw will loosen (Schwarz 2000).
Eccentric and compressive forces generated by chewing movements reduce the preten-sion on the screw, reducing its retention (Dixon et al. 1995; Binon 1996; Gratton et al. 2001; Siamos et al. 2002; Khraisat et al. 2004; Akour et al. 2005; Kitagawa et al. 2005; Yousef et al. 2005). This situa-tion seems to be in direct contrast to im-plants with internal tapered connections; the fixation and the stability of these systems are not a function of the screw, but rather conferred by the frictional resis-tance resulting from the contact between the conical mating parts of the abutment and the implant.
Mathematical formulas and finite element models have shown that over 86% of the tightening torque and over 98% of the loosening torque are balanced by the tapered section of these systems (Bozkaya & Mu ̈ftu ̈ 2005). The frictional resistance resulting from the contact of the conical mating parts of tapered joints in-creases with the application of axial com-pressive forces (Bozkaya & Mu ̈ftu ̈ 2003).
However, the extent into which bending moments and upward tensile loads result-ing from eccentric dynamic occlusal forces interfere negatively with the abutment retention is not certainly known. Repeated screw tightening is also a con-cern when fabricating an implant-supported restoration (Al Rafee et al. 2002).
The installation torque value specified for a common screw joint is valid only for the initial assembly of the fastener; continued use of the same screw tends to alter and change the coefficient of friction properties of the joint, resulting in a lower preload in the screw after as few as five installations (Parmley 1989). This author reported that, after 10 installations, preload loss can range as much as 30% to 60%.
Consecutive impression and try-in procedures may cause wearing of the components, decreasing the coefficient of friction between the mating components and weakening the nion between the implant and the abutment (Weiss et al. 2000). Byrne et al. (2006) tested three types of screws under repeated tigh-tening at 10, 20 and 30 N cm, and found that all screw types displayed some decay in the preload with repeated tightening.
Weiss et al. (2000) studied seven different types of implant/abutment assemblies in up to 200 insertion/removal cycles, and reported that repeated insertion/removal cycles caused progressive loss of torque retention in all systems, probably due to a decrease in the coefficient of friction between the mating components. These authors also concluded that, mong the systems tested, the ones that consistently maintained the highest opening torque values contained tapered frictional elements. One study reported that the repeated use of a saliva-lubricated gold prosthetic retaining screw achieved higher preload values (Tzenakis et al. 2002); the method used in this study is questionable, though, because only one im- plant and one abutment were used through-out the study to test 45 screws of three different types.
The purpose of this study was to evalu-ate the short-term influence of the com-pressive, tensile and oblique loads generated by simulated occlusal move-ments on the torque loss of abutments with internal tapered connections, compar-ing the torque loss of loaded and unloaded abutments. This study also evaluated the effect of repeated insertion/removal ycles on the removal torque of these abutments.
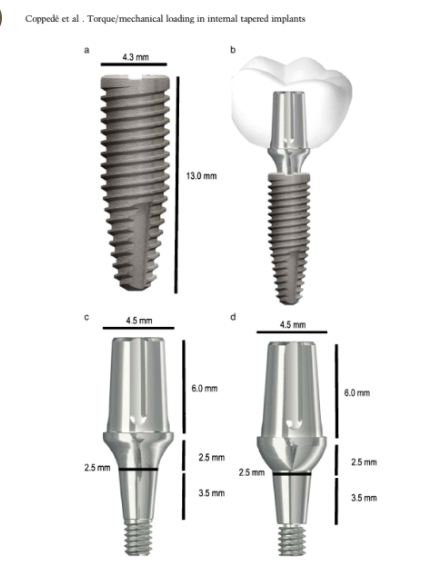
Two types of abutments with internal tapered connections were evaluated: a solid abutment, with a threaded apical portion, and a two-piece abutment, with a transfix-ing screw. Material and methods This study utilized 68 conical implants Alvim CM (Neodent Implante Osseointe-gra ́vel, Curitiba, Brazil), with an 11.51, 3.5 mm height and a 2.5-mm-diameter internal tapered connection. The implant external dimensions were 4.3 mm dia-meter and 13 mm length (Fig. 1a), and a schematic prospective restoration is shown (Fig. 1b). Two abutment types were used:
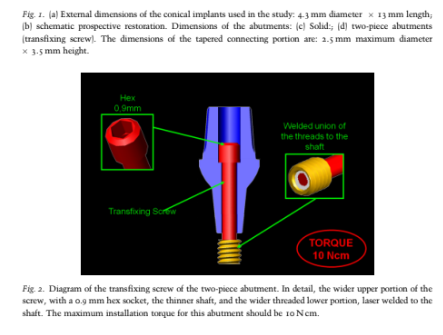
Universal Abutment CM (Neodent Im-plante Osseointegra ́vel), a one-piece solid abutment, with an apical threaded portion, with 4.5 mm diameter, 2.5 mm neck and 6 mm height Fig. 1c); and a Universal Abutment CM Transfixing Screw (Neodent Implante Osseointegra ́vel), a two-piece abutment transfixed by a screw, with dimensions of 4.5 mm diameter, 2.5 mm neck and 6 mm height (Fig. 1d). The threaded portion of the transfixing screw is laser welded to the shaft after the screw is inserted through the abutment. The type of screw utilized in this implant system is ISO M1.80, and the recommended insertion torque is 10 N cm (Fig. 2). Both types of abutments are indicated for cemented restorations. Thirty-four abut-ments of each type were used. All implants and abutments were delivered from com-mercially available stock.
The implants and abutments were divided into four groups with 17 implant/abutment assemblies each: groups 1 and 3 received the one-piece solid abutments, while groups 2 and 4 received the two-piece abutments. Groups 3 and 4 were mechanically loaded and groups 1 and 2 were not. During the tests, two-piece abutments loaded mechani-cally (group 4) were frictionally locked to the implants. The torque-out action of this kind of abutment presented two distinct moments: first, a certain amount of reverse.
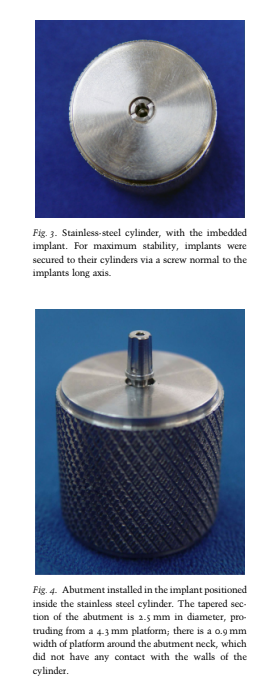
torque was necessary to loosen the fixation screw; then, a higher amount of reverse torque was necessary to remove the locked abutment from the implant. Torque-out va-lues of the implant/abutment assemblies of group 4 were collected in these two distinct moments, and catalogued under two sub-groups: 4a (reverse torque value that loo-sened the screw) and 4b (reverse torque necessary to remove the abutment from the implant). Thus, subgroups 4a and 4b were two different measurements collected from the same implant/abutment assemblies of group 4. Groups 1 and 2 were used as control groups. The implants were imbedded in a 26 mm diameter 24.5 mm height stain-less-steel cylinder with internal walls that matched implant external dimensions. For maximum stability, implants were secured to their cylinders via a screw normal to the implants long axis. The surgical protocol for these implants recommends an installa- tion depth of 1–3 mm below the bone crest.
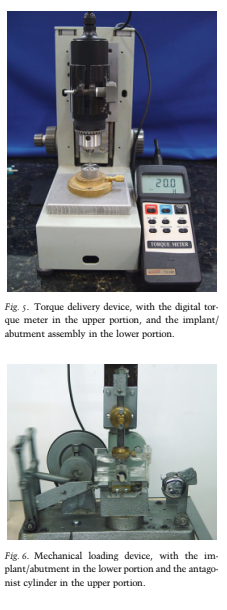
In this study, implant platforms were posi-tioned 1 mm below the top of the stainless-steel cylinders (Fig. 3). The tapered section of the abutment is 2.5 mm in diameter, protruding from a 4.3 mm platform; there is always a 0.9 mm width of platform around the emergence of the abutment neck, and hence the neck of the abutments did not have any contact with the walls of the cylinder, protruding with any interfer-ence (Fig. 4).
The cylinder with the imbedded implant was positioned at the base of a torque delivery device, developed by the Depart-ment of Dental Materials and rostheses of the School of Dentistry of Ribeira ̃o Preto, University of Sa ̃o Paulo. In the upper por-tion of this device, a digital torque meter was installed (TQ-680, Instrutherm, Sa ̃o Paulo, Brazil). The abutments were in-stalled in the respective implants with the insertion torque recommended by the man-ufacturer, which was 20 N cm for the solid abutments and 10 N cm for the two-piece abutments. Torque-in values were mea-sured with the digital torque meter, with decimal precision (Fig. 5). After 5 min, the abutments were uninstalled, and torque-out values were measured. Ten insertion/ removal cycles were performed for each implant/abutment assembly; insertion and removal torque values were recorded in each of the 10 cycles.
Groups 3 and 4 (a and b) were used as test groups. The abutments were installed in the implants in the same manner as detailed for groups 1 and 2.
Torque-in values were measured with the digital tor-que meter. Five minutes after installation, the cylinder with the implant/abutment assembly was placed in a mechanical load-ing device, developed by the Department of Dental Materials and Prostheses of
the School of Dentistry of Ribeira ̃o Preto, University of Sa ̃o Paulo, which simulates masticatory movements (Fig. 6). In this device, an electrical motor moves a lever arm with a 265 cycles/min speed. An
acrylic recipient is attached to the lever arm of the device, and performs a 10 mm course, resulting in a linear speed of 88 mm/s.
The implant/abutment assem-bly was installed inside the acrylic recipi-ent. Over the acrylic recipient, there is a pole with a vertical adjustment; when released, the pole was allowed to rest over the implant/abutment assembly.
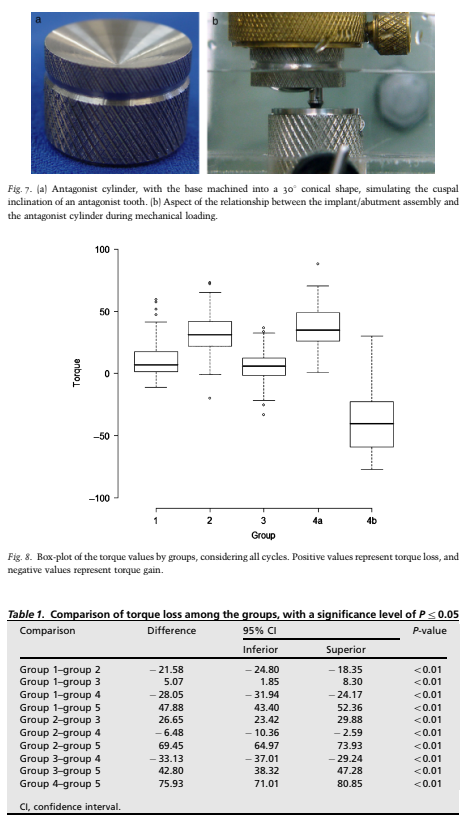
A 26 mm diameter 18.2 mm height stainless-steel cylinder was prepared to be installed in the lower tip of the pole; the base of the cylinder was machined into a 301 conical shape, simulating the cuspal inclination of an antagonist tooth (Fig. 7a). Once the pole was completely released, a total weight of 553 g was applied over the im-plant/abutment assembly. During the tests, the implant/abutment assemblies and the antagonist device were completely submerged in deionized water (Fig 7b).
This mechanical loading device was de-signed according to the norm ISO/TS 14569-2 (Dental Materials – Guidance on testing of wear – Part 2: Wear by two – and/or three body contact, 2001) under the Freiburg Method. Each mechanical loading test was carried out for 15 min, performing a total of 1.325 cycles, which corresponded to 3–4 days of normal oral function (Gateau et al. 1999). After mechanical loading, abutments were uninstalled from the implants, and torque-out values were measured. Ten insertion/removal cycles were performed per sample; insertion and removal torque values were recorded in each of the 10 cycles.
The relative values were obtained, calculating the percentage of the removal torque in relation to the insertion torque. When removal torque was lower than insertion torque, the percentage was ex-pressed with a positive value, and when removal torque was higher than insertion torque, the percentage was expressed with a negative value. This calculation was performed for all values collected in each of the 10 cycles, resulting in an indepen-dent relative value for each cycle, for all samples tested. The statistical analysis was performedutilizing a mixed linear model, which is a generalization of the standard linear model (ANOVA). This model is used in the ana-lysis of data in which the responses of the same specimen are grouped, and the as-sumption of independence among the observations in the same group is not adequate (Schall 1991).
For the utilization of this model, it is necessary that the errors have a normal distribution with mean zero and constant variance. The comparisons were performed utilizing contrast, testing the linear function of the parameters. The adjustment of the model was carried out with the procedure PROC MIXED of the software SAS 9.1(SAS Institute Inc., Cary, NC, USA). Scanning electron microscopy and optical microscopy All abutments were analyzed, before and after complete testing, in a scanning elec-tron microscope (EVO 50, Carl Zeiss, Oberkochen, Germany), and photomicro-graphs were obtained at 40 and 80.
One implant/abutment assembly from each group was removed from the test after the completion of the first cycle, and another implant/abutment assembly was removed from each group after the completion of the 10th cycle. These implant/abutment as-semblies were imbedded in polystiren resin, longitudinally sectioned and analyzed in a scanning electron microscope (DSM 960, Carl Zeiss). Photomicrographs were obtained at 10 magnification. These implant/abutment assemblies were also analyzed in an optical microscope (Neophot 30, Jena-Carl Zeiss, Gena, Germany), and photographed with a digital color camera (CC-8703, GKB, Tai Chung, Taiwan).
Results
The two-piece abutments showed different behaviors in groups 2 and 4. In group 2, the installation torque of 10 N cm recom-mended for these abutments was not en-ough to induce efficient frictional locking of the abutments into the implants; there-fore, when the screws were loosened, the abutments came apart from the implants. For group 4, after mechanical loading, the abutments were frictionally locked into the implants. A certain amount of reverse torque was necessary to loosen the screws, but the abutments continued attached to the implants. A continued application of reverse torque was necessary until the lower head of the screws engaged the base of the abutments, and a higher torque-out value was necessary to push out the abut-ments, and disassemble them from the implants.
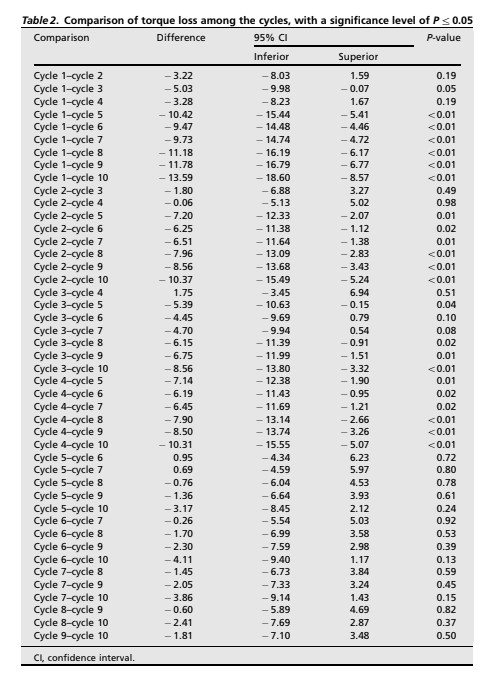
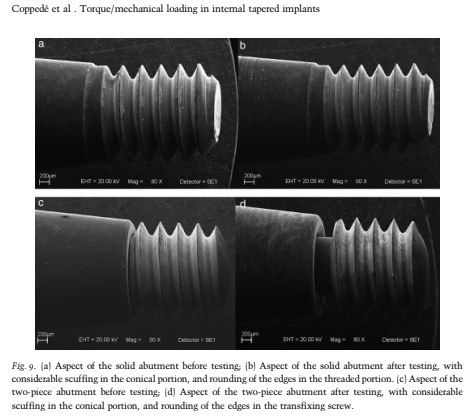
These two torque-out values were recorded under two subgroups: 4a, in which the torque-out values represented the reverse torque necessary to loosen the screw; and 4b, in which the torque-out values represented the reverse torque necessary to remove the abutment from the implant. Data distribution among the groups is shown in Fig. 8. Torque loss was higher in groups 4a and 2, which presented over 30% loss; group 1 showed a 10.5% torque loss; group 3 presented a 5.4% torque loss; and group 4b showed a 39% torque gain. A statistical comparison is shown in Table 1. All the results were significantly different; group 4b showed torque gain. The other groups showed different amounts of torque loss. Among these groups, higher relative torque-out values were obtained by group 3, followed by groups 1, 2 and 4a.
torque-out values tended to be lower, for all abutment types. In group 4 (a and b), some of the samples were removed from the tests because of screw fractures. The screws of ten out of the 17 abutments of this group fractured while ttempting to remove the abutment from the implant after mechanical loading.
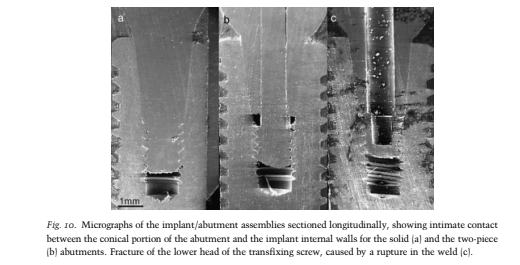
Scanning electron miscroscopy Comparison of the micrographs of the abutments before and after 10 insertion/removal cycles revealed considerable scuff-ing, creating horizontal lines in the conical portion of the abutments, and rounding of the edges of their threaded portion, char-acterizing the mechanical wear of the abut-ments after the test cycles, as shown in Fig. 9a–d. The micrographs of the implant/abutment assemblies sectioned longitu-dinally showed intimate contact between the conical portion of the abutment and the implant internal walls, both for the solid and for the two-piece abutments (Fig. 10a and b).
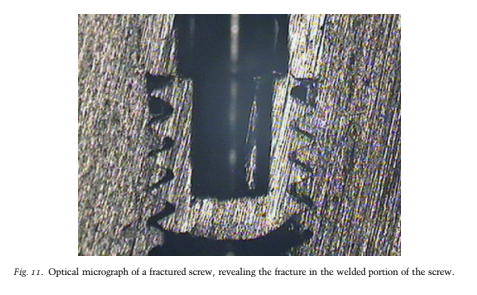
Micrographs of the implant/abutment assemblies with screw fractures in group 4 showed that the fractures always occured on the lower head of the screws, caused by a rupture in the weld between the threads and the shaft of the screws (Fig. 10c). Optical microscopy Optical micrographs of the implant/abut-ment assemblies confirmed the findings of scanning electron microscopy. Images
of the fractured screws revealed that the fractures always occurred in their welded portion (Fig. 11).
Discussion
The dual nature of the mechanics of tapered connections cannot be neglected; both the screw and the conical mating parts of the abutment and the implant act together in the insertion and in the removal process of the abutments, both for the solid and for the two-piece abutments. Most of the fixation of these systems is not performed by the screw, but rather by the frictional resistance resulting from the con-tact between the mating tapered sections.
Bozkaya and Mu ̈ftu ̈ (2005) have demon-strated with mathematical formulas that over 86% of the tightening torque and over 98% of the loosening torque are balanced by the tapered section of internal tapered connection systems. In this study, it was not possible to distinguish the torque va-lues of the screw from those of the tapered section when using solid abutments, because they are one-piece components.
For the two-piece abutments, however, this discrimination was possible, and the results of group 4 were categorized into two subgroups: 4a and 4b. These groups were separated for analytical purposes only, because both values are fractions of the same torque-out process. Even though occlusal movements gener-ate bending moments and upward tensile loads that may interfere negatively with the retention of the abutment, the axial compressive component of occlusal forces acts in the direction of abutment insertion, which increases contact pressure and frictional resistance (Sutter et al. 1993; Bozkaya & Mu ̈ftu ̈ 2003).
The results of the present study corroborate these infer-ences, because mechanically loaded abutments showed an increase in the tor-que-out values compared with unloaded abutments, most likely because the effects of the axial compressive component of the simulated occlusal loading surpassed the effects of the other oblique and tensile forces.
In this study, all abutments that were not loaded (groups 1 and 2) presented some torque loss, which is in agreement with the findings of Norton (1999). Solid abutments (group 1) presented 10.5% torque loss and two-piece abutments (group 2) presented 32% torque loss. In group 2, no effective frictional locking occurred with the instal-lation torque of 10 N cm, and the loosening of the screws alone released the abutment. However, mechanically loaded abutments seemed to show an increase in their reten-tion, with superior loosening torques com-pared with the unloaded abutments.
Loaded solid abutments (group 3) presented 5.4% torque loss, which represents a sig-nificant reduction in torque loss compared with group 1 (10.5%). Loaded two-piece abutments (group 4) presented two distinct situations: group 4a (torque necessary to loosen the screw) presented 37.2% torque loss; although significantly different from the results of group 2 (32%), the similarity of these results suggests that the loosening of the fixation screws was hardly influ-enced by the eccentric forces generated by simulated occlusal loading, possibly due to the mechanical stability provided by the tapered connection. However, group 4b (torque necessary to remove the abutment from the implant) presented a 39% torque gain, which represents a significantly bet-ter result compared with group 2 (32% torque loss).
These findings suggest that, under simulated occlusal loading, the tapered portion of the two-piece abutments increases contact pressure and frictional resistance with the mating part of the implant without any interference from the transfixing screw, and they become frictionally locked. Torque gain did not occur with solid abutments under mechanical loading, pos-sibly because its apical threaded portion did not allow full compression of the tapered portion of the abutment into the mating part of the implant, reducing the potential contact pressure. Nevertheless, torque-out values for loaded solid abutments were higher than those for unloaded solid abut-ments, which demonstrated that the simulated occlusal loading, even with the limitation imposed by the apical threaded portion, resulted in an effective increase of the contact pressure of the tapered mating parts.
The design of the retention screw for the two-piece abutments presents two wider portions: the upper and the lower heads. When the screw is tightened, the upper head contacts the base of the screw housing inside the abutment, approximating the abutment to the implant. The shaft of the screw has a reduced diameter, so that the abutment walls can be thick enough to resist functional loads. The lower threaded head is meant to engage the negative threads in the interior of the implant, which are wider than the shaft of the screw. Thus, the lower threads have to be laser welded to the shaft after it is inserted through the abutment in the fabrication process (Fig. 2).
During the tests of group 4, the screws were torqued out until their lower threaded head engaged the bottom of the abutment, and were utilized to remove the abutments that were frictionally locked into the implants after mechanical loading. On doing this, 10 out of 17 screws frac-tured. Scanning electron and optical micro-graphs showed that the fractures always occurred in the welded portion of the screws (Fig. 8). These results suggest that the screw should not be used to remove the abutment after installation in clinical use; its only function should be to bring the components together during installa-tion. Like in other internal tapered connec-tion systems, if removal of the abutment is necessary, an external device capable of applying a rotational force on the abutment should be used to remove frictionally locked abutments from the implants, after complete loosening of the screw.
Consecutive insertion/removal cycles seem to have a deleterious effect on theunion between the implant and the abut-ment in various implant connection sys-tems (Parmley 1989; Weiss et al. 2000; Byrne et al. 2006). The findings of this study suggest that repeated insertion/removal cycles of abutments with 11.51 internal tapered connections also have a negative impact over their retention. Scan-ning electron micrographs showed consid-erable scuffing on the conical portion of the abutments, and rounding of the edges on their threaded portion, which suggest mechanical wear of these abutments after cycling.
Based on these findings, it is advisable that abutments with internal tapered connections should not be removed after installation, unless strictly necessary. The load used in the mechanical loading of the implant/abutment assemblies in groups 3 and 4 was 553 g, which corre-sponds approximately to 5 N. This value is representative of a limitation of this study, because it is rather low compared with normal occlusal forces, which can be higher than 100 N. Even with this limited load, simulated occlusal movements ex-erted a positive effect on over the assem-blies, reducing the torque loss of the abutments.
Another limitation of this study was the number of simulated chew-ing cycles, which represented 3–4 days of normal oral function. However, this limited number of cycles was sufficient to promote an increase in the retention of the loaded abutments compared with unloaded ones, which suggests that the masticatory movements have a short-term beneficial effect over the retention of these abut-ments.
Further studies are necessary to verify the effects of higher loads and a greater number of cycles on the long-term retention and stability of abutments with internal tapered connections. Conclusion Within the limitations of this in vitro study, the following conclusions were drawn:
- Short-term mechanical loading of abutments with internal tapered connections increased their loosening torque when compared with similar
- abutments that were not mechanically loaded.
- Only loaded two-piece abutments showed torque gain, with torque-out values higher than torque-in values.
- The transfixing screws of the two-piece abutments should not be used to remove frictionally locked abutments from the implants; most of the screws fractured on attempting todo this. Removal torque values tended to de-crease as the number of insertion/
- removal cycles increased.
- Acknowledgements: The authors
- would like to acknowledge Neodent
- Implante Osseointegra ́ vel (Curitiba,
- Brazil) for providing the implants and
- implant components and the National
- Council for Scientific and Technological
- Development (CNPq) for the financial
- support.
References
Aboyoussef, H., Weiner, S. & Ehremberg, D. (2000) Effect of an antirotation resistance form on screw loosening for single implant-supported crowns. Journal of Prosthetic Dentistry 83: 450–455. Akour, S.N., Fayyad, M.A. & Nayfeh, J.F. (2005) Finite element analyses of two antirotational designs of implant fixtures. Implant Dentistry 14: 77–81. Al Rafee, M.A., Nagy, W.W., Fournelle, R.A., Dhuru, V.B., Tzenakis, G.K. & Pechous, C.E. (2002) The effect of repeated torque on the ultimate tensile strength of slotted gold prosthetic screws. Journal of Prosthetic Dentistry 88: 176–182. Binon, P.P. (1996) The effect of implant/abutment hexagonal misfit on screw joint stability. Interna-tional Journal of Prosthodontics 9: 149–160. Boggan, R.S., Strong, J.T., Misch, C.E. & Bidez, M.W. (1999) Influence of hex geometry and prosthetic table width on static and fatigue strength of dental implants.
Journal of Prosthetic Dentistry 82: 436–440. Bozkaya, D. & Mu ̈ftu ̈ , S. (2003) Mechanics of the tapered interference fit in dental implants. Journal of Biomechanics 36: 1649–1658. Bozkaya, D. & Mu ̈ftu ̈ , S. (2005) Mechanics of the taper integrated screwed-in (TIS) abutments used in dental implants.
Journal of Biomechanics 38: 87–97. Byrne, D., Jacobs, S., O’Connel, B., Houston, F. & Claffey, N. (2006) Preloads generated with re-peated tightening in three types of screws used in dental implant assemblies. Journal of Prostho-dontics 15: 164–171. Carrilho, G.P.B., Dias, R.P. & Elias, C.N. (2005) ‘Comparison of external and internal hex im-plants’ rotational freedom: a pilot study. Interna-tional Journal of Prosthodontics 18: 165–166. C ̧ ehreli, M.C., Akc ̧a, K., Iplikc ̧ioglu, H. & Sahin, S. (2004) Dynamic fatigue resistance of implant-abutment junction in an internally notched morse-taper oral implant: influence of abutment design.
Clinical Oral Implants Research 15: 459–465. Cho, S.C., Small, P.N., Elian, N. & Tarnow, D. (2004) Screw loosening for standard and wide diameter implants in partially edentulous cases: Coppedeˆ et al . Torque/mechanical loading in internal tapered implants c 2009 The Authors. Journal compilation c 2009 John Wiley & Sons A/S 631 | Clin. Oral Impl. Res. 20, 2009 / 624–632 3- to 7- year longitudinal data. Implant Dentistry 13: 245–250. Dixon, D.L., Breeding, L.C., Sadler, J.P. & McKay, M.L. (1995) Comparison of screw loosening, rota-tion and deflection among three implant designs.
Journal of Prosthetic Dentistry 74: 270–278. Gateau, P., Sabek, M. & Dailey, B. (1999) Fatigue testing and microscopic evaluation of post and core restorations under artificial crowns. Journal of Prosthetic Dentistry 82: 341–347. Goodacre, C.J., Kan, J.I.K. & Rungcharassaeng, K. (1999) Clinical complications of osseointegrated implants.
Journal of Prosthetic Dentistry 81: 537–552. Gratton, D.G., Aquilino, S.A. & Stanford, C.M. (2001) Micromotion and dynamic fatigue proper-ties of the dental implant-abutment interface. Journal of Prosthetic Dentistry 85: 47–52. Henry, P.J., Laney, W.R., Jemt, T., Harris, D., Krogh, P.H.J., Polizzi, G., Zarb, G.A. & Herr-mann, I. (1996) Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study.
International Journal of Oral & Maxillofacial Implants 11: 450–455. Khraisat, A., Hashimoto, A., Nomura, S. & Miya-kawa, O. (2004) Effect of lateral cyclic loading on abutment screw loosening of an external hexagon implant system. Journal of Prosthetic Dentistry 91: 326–334. Khraisat, A., Stegaroiu, R., Nomura, S. & Miya-kawa, O. (2002) Fatigue resistance of two im-plant/abutment joint designs.
Journal of Prosthetic Dentistry 88: 604–610. Kitagawa, T., Tanimoto, Y., Odaki, M., Nemoto, K. & Aida, M. (2005) Influence of implant/abutment joint designs on abutment screw loosening in a dental implant system. Journal of Biomedical Materials Research Part B: Applied Biomaterials 75B: 457–463. Maeda, Y., Satoh, T. & Sogo, M. (2006) In vitro differences of stress concentrations for internal and external hex implant-abutment connections: a short communication. Journal of Oral Rehabi-litation 33: 75–78.
Mangano, C. & Bartolucci, E.G. (2001) Single tooth replacement by morse taper connection implants: a retrospective study of 80 implants. International Journal of Oral & Maxillofacial Implants 16: 675–680. Merz, B.R., Hunenbart, S. & Belser, U. (2000) Mechanics of the implant-abutment connection: an 8-degree taper compared to a butt joint con-nection. International Journal of Oral & Max-illofacial Implants 15: 519–526.
Norton, M.R. (1997) An in vitro evaluation of the strength of an internal conical interface compared to a butt joint interface in implant design. Clinical Oral Implants Research 8: 290–298. Norton, M.R. (1999) Assesment of cold welding properties of the internal conical interface of two commercially available implant systems. Journal of Prosthetic Dentistry 81: 159–166. Parmley, R.O. (1989) Standard Handbook of Fastening and Joining. 2nd edition, p. 1–25. New York: McGraw-Hill.
Schall, R. (1991) Estimation in generalized linear mod-els with random effects. Biometrika 78: 719–727. Schwarz, M.S. (2000) Mechanical complications of dental implants. Clinical Oral Implants Research 11 (Suppl.): 156–158. Siamos, G., Winkler, S. & Boberick, K.G. (2002) The relationship between implant preload and screw loosening on implant-supported prostheses. Journal of Oral Implantology 28: 67–73. Sutter, F., Weber, H.P., Sorensen, J. & Belser, U. (1993) The new restorative concept of the ITI dental implant system: design and engineering.
International Journal of Periondtics and Restora-tive Dentistry 13: 409–431. Tzenakis, G.K., Nagy, W.W., Fournelle, R.A. & Dhuru, V.B. (2002) The effect of repeated torque and salivary contamination on the preload of slotted gold implant prosthetic screws. Journal of Prosthetic Dentistry 88: 183–191. Weiss, E.I., Kozak, D. & Gross, M.D. (2000) Effect of repeated closures on opening torque values in seven abutment-implant systems. Journal of Pros-thetic Dentistry 84: 194–199. Yousef, H., Luke, A., Ricci, J. & Weiner, S. (2005) Analysis of changes in implant screws subject to occlusal loading: a preliminary analysis. Implant Dentistry 14: 378–385.
Abı ́lio Ricciardi Coppedeˆ
Maria da Glo ́ria Chiarello de
Mattos
Renata Cristina Silveira
Rodrigues
Ricardo Faria Ribeiro
Authors’ affiliations:
Abı ́lio Ricciardi Coppedeˆ, Maria da Glo ́ria Chiarello de Mattos, Renata Cristina Silveira Rodrigues, Ricardo Faria Ribeiro, Department of Dental Materials and Prostheses, School of Dentistry of Ribeira ̃o Preto, University of São Paulo, Ribeira ̃o Preto, São Paulo, Brazil
Correspondence to: Dr. Ricardo Faria Ribeiro Department of Dental Materials and Prostheses, School of Dentistry of Ribeira ̃o Preto, University of Sa ̃o Paulo Avenida do Cafe ́, s/n, Monte Alegre CEP: 14040-904 Ribeira ̃o Preto, São Paulo Brazil
Tel: þ 55 (16) 3602 4005
Fax: þ 55 (16) 3602 0999
e-mail: rribeiro@forp.usp.br
