Mechanical Comparison of Experimental Conical-Head Abutment Screws with Conventional Flat-Head Abutment Screws for External-Hex and Internal Tri-Channel Implant Connections: An In Vitro Evaluation of Loosening Torque
Abílio Ricciardi Coppedê, DDS, PHD1/Adriana Cláudia Lapria Faria, DDS, PHD2/Maria da Glória Chiarello de Mattos, DDS, PHD3/Renata Cristina Silveira Rodrigues, DDS, PHD4/Jamil Awad Shibli, DDS, PHD5/Ricardo Faria Ribeiro, DDS, PHD3
Purpose: This study compared the loosening torque of experimental conical-head abutment screws to that of conventional flat-head screws of implants with external-hex (EH) and internal tri-channel (IT) connections before and after mechanical loading. Materials and Methods: Forty-four implant/screw/abutment assemblies were divided into four groups: EH/flat-head screw (EH), IT/flat-head screw (IT), EH/conical-head screw (EHCS), and IT/conical-head screw (ITCS). Three assemblies from each group were analyzed in a stereoscopic magnifier and then returned to their respective groups.
One assembly was removed from each group and transversely sectioned for optical microscopy analysis. Abutments were tightened at 32 Ncm of torque; after 10 minutes, loosening torque was measured. The same abutments were then retightened with 32 Ncm of torque; after 10 minutes, they were mechanically loaded for 300,000 cycles and loosening torque was again measured. Data were collected and an exploratory analysis was performed.
Comparisons were made by orthogonal contrasts using a linear mixed effects model (random and fixed effects). Results: Comparisons before mechanical cycling showed significant differences between groups except for EH vs IT and EHCS vs ITCS. After mechanical cycling, only the comparisons EH vs IT and EHCS vs ITCS showed no significant differences. Considering the same group, before and after mechanical cycling, all comparisons showed significant differences.
Conclusions: The shape of the abutment screw head significantly influenced loosening torque: conical-head screws showed higher loosening torque values than conventional flat-head screws before and after loading. The implant/abutment connection design exerted no significant influence on loosening torque. I nt J ORal MaxIllOfac IMplants 2013;28:e321–e329. doi: 10.11607/jomi.3029.
Key words: conical abutment screw, dental implants, implant- upported prostheses, loosening torque, tightening torque
1- Former Postgraduate Student, Department of Dental Material sand Prostheses, School of Dentistry of Ribeirão Preto, University of São Paulo, Ribeirão Preto, São Paulo, Brazil.
2- Laboratory Specialist, Department of Dental Materials and Prostheses, School of Dentistry of Ribeirão Preto, University of São Paulo, Ribeirão Preto, São Paulo, Brazil.
3- Full Professor, Department of Dental Materials and Prostheses, School of Dentistry of Ribeirão Preto, University of São Paulo, Ribeirão Preto, São Paulo, Brazil.
4- Assistant Professor, Department of Dental Materials and Prostheses, School of Dentistry of Ribeirão Preto, University of São Paulo, Ribeirão Preto, São Paulo, Brazil.
5- Professor, Department of Periodontology, University of Guarulhos, Guarulhos, Brazil.
Correspondence to: Dr Ricardo Faria Ribeiro, Department of Dental Materials and Prostheses, School of Dentistry of Ribeirão Preto, University of São Paulo, Avenida do Café, s/n, Monte Alegre, CEP: 14040-904 Ribeirão Preto, São Paulo, Brazil. Fax: +55-16-3602-4780. Email: rribeiro@forp.usp.br ©2013 by Quintessence Publishing Co Inc.
The original implant/abutment joint design for utilization in full-arch prostheses was a butt joint medi-ted by an external hexagon,1,2 and high success ratesand few mechanical problems were reported. However, mechanical problems started to occur when single-tooth restorations were initially connected using this type of joint. Lack of stability of the screwed joint, screw loosening, and fracture were the most significant mechanical drawbacks reported. 3–7 In these early stages of single-tooth implant-supported restorations, abutment screws were made with low-resistance alloys, the slotted engagement was notideal for delivering adequate tightening torque levels, and devices to measure torque were not available. 3–10 These adversities led to several evelopments in the components and materials of the screw joint. Torque-delivering devices were created to make the implant/abutment connection more stable. More Coppedê et ale322 Volume 28, Number 6, 2013 precise antirotational mechanisms were developed.
Machining tolerances were improved. Abutment screws were made of more resistant alloys, with more refined surfaces and sometimes with surface coating materials to reduce friction and increase preload. New types of screwdriver engagements were introduced to allow the application of higher torque values, such as the hexagonal, square, and unigrip engagement designs. Torque measurement devices were created so that the torque applied to the screw could be calibrated to obtain the ideal preload. 8,11–27 These improvements considerably reduced the occurrence of screw loosening in single-tooth restorations.
More recent studies have suggested that screw loosening, regardless of the implant/abutment connection used, is now an uncommon clinical complication.17–22,25 Conical connections were developed to improve the mechanical properties of joints in general. These connections provide a friction- ocking mechanism between the mating parts of the joint to improve stability. 28 Comparative in vitro studies and finite element analyses have demonstrated that conical implant/abutment connections present higher static and dynamic resistance 9,29,30 and higher resistance to screw loosening 31 than other connections.
For the present study, an experimental abutment screw with a conical head was designed to create a friction-locking mechanism between the screw head and the abutment internal mating part. The objective of this conical-head screw was to reduce screw loosening and preserve preload, regardless of the type of implant/abutment connection. The friction-locking mechanism between the screw and the abutment was meant to improve the resistance of the screw to rotational micro-movements during function, thus preserving the preload.
However, to date, there is no scientific evidence of the efficacy of conical-head abutment screws in implant-supported single restorations. The purpose of this study, therefore, was to compare the effects of in vitro mechanical loading on the loosening torque of experimental conical-head abutment screws and of conventional flat-head screws on implants with external-hex (EH) and internal tri-channel (IT) connections. The postulated null hypothesis was that neither the shape of the head of the abutment screw nor the type of connection would influence loosening torque after mechanical loading simulating 1 year of oral function.
Material and Methods
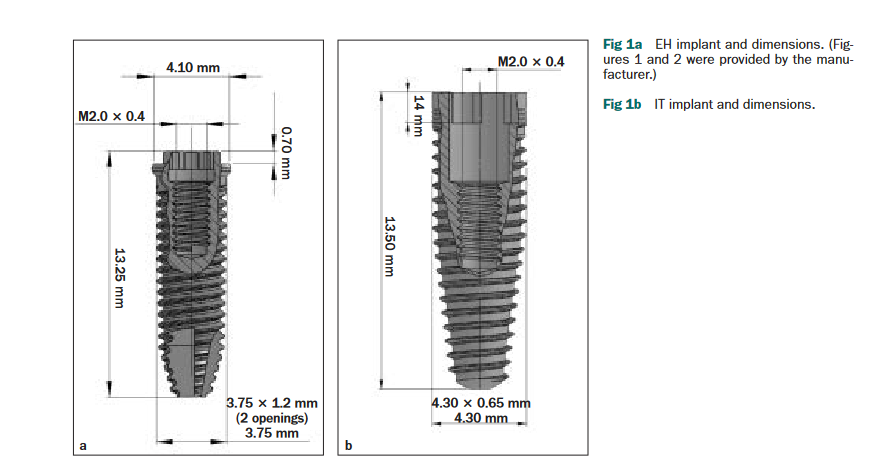
Forty-four implants were produced for this investigation. Twenty-two implants had an EH connection (Dérig), cylindric macrogeometry, diameter of 3.75 mm, length of 13.25 mm, platform diameter of 4.1 mm, hex height of 0.7 mm, hex diameter of 2.7 mm, 3.75- × 1.2-mm external threads, and 2.0- × 0.4-mm internal threads (Fig 1a). The other 22 implants featured an IT connection (Dérig), conical macrogeometry, diameter of 4.3 mm, length of 13.50 mm, collar of 1.4 mm, 4.30- × 0.65-mm external threads, and 2.0- × 0.4-mm internal threads (Fig 1b). All implants were made with grade 4commercially pure titanium (American Society for Test- ing Materials [ASTM] F67).
Forty-four abutment screws were produced with titanium-aluminum-vanadium alloy (Ti-6Al-4V) (ELI, ASTM F136, Dérig). Twenty- wo were conventional flathead screws—11 for the EH-connection implants and 11 for the IT-connection implants (Figs 2a and 2b)
and 22 were experimental conical-head screws—11 for EH-connection implants and 11 for IT-connection implants (Figs 2c and 2d). Forty-four abutments for single-tooth prostheses were then produced in Ti-6Al-4V (ELI, ASTM F136, Dérig) for the respective connection types and screw designs. All implants, abutments, and screws were fabricated by only one manufacturer exclusively for experimental use in this investigation.
The implant/abutment/screw assemblies were divided into four different groups.
• EH: 11 assemblies with EH connections and conventional flat-head screws
• IT: 11 assemblies with IT connections and conventional flat-head screws
• EHCS: 11 assemblies with EH connections and experimental conical-head screws
• ITCS: 11 assemblies with IT connections and experimental conical-head screws
Before the tests, three implant/screw/abutment assemblies from each group were randomly selected for nondestructive initial optical microscopic analysis.
These analyses were made in a stereoscopic magnifier (model S8AP0, Leica Microsystems) at standardized magnifications of ×16, ×20, ×25, and ×40. After this, the specimens were returned to their respective groups. One assembly was permanently separated from each group for destructive analysis. These were embedded in transparent acrylic resin and transversely sectioned for optical microscopy analysis. The microscope featured specific software that allowed for image capture (Leica Application Suite, Version 3.4.1, Leica Microsystems).
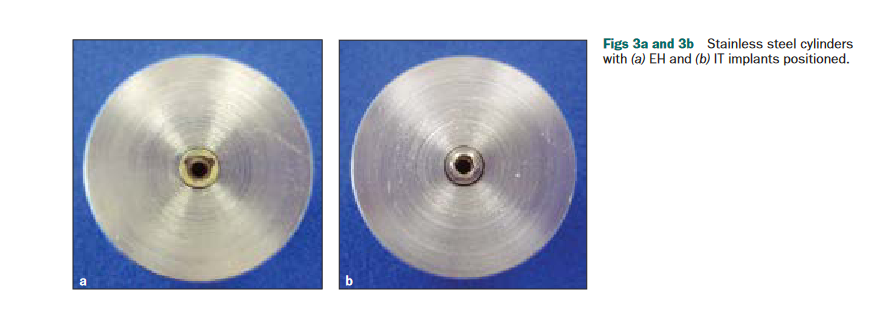
Ten stainless steel cylinders, 26 mm in diameter and 20 mm in length, were perforated in the center of the flat surface; five EH cylinders had 4.1-mm-diameter perforations and five IT cylinders had 4.3-mm perforations. All perforations were 15 mm deep and parallel to the long axis. A lateral hole was created to fit a transverse fixation screw. The implants were then press-fit inside the cylinders up to their platform surfaces, which granted them considerable stability against lateral and rotational movements. The fixation screws were tightened to ensure that the implants were absolutely stable and to obtain complete final locking of the implants against lateral and rotational movements (Figs 3a and 3b).
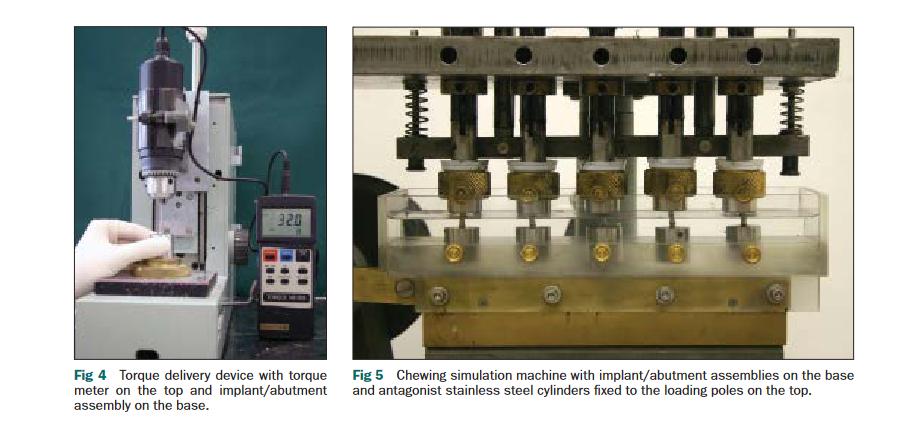
To measure initial tightening and loosening torques (t0), a digital torque meter (TQ-680, Instrutherm) was positioned in a torque measuring device (Department of Dental Materials and Prostheses, School of Dentistry of Ribeirão Preto, University of São Paulo). The torque meter was positioned on the top of the device, and the implant/screw/abutment assembly embedded in the steel cylinder was positioned on the bottom of the device, in a socket that allowed only rotational movement of the cylinder (Fig 4). All abutments were tightened to their respective implants with 32 Ncm of torque. Aftera 10-minute interval, loosening torque was measured and recorded.
For mechanical loading tests (t1), all implant/screw/abutment assemblies were retightened to 32 Ncm. After a 10-minute interval, they were positioned in a chewing simulation machine (Department of Dental Materials and Prostheses, Dental School of Ribeirão Preto, University of São Paulo) (Fig 5). A similar machine had been described in a previous study 30 and had a maximum loading capacity of 5 N. The machine developed for the present study was designed to function with a maximum load of 50 N, similar to masticatory forces in posterior regions. 20,32–35 In this machine, a 0.5-hp, 1,720-rpm motor with an adjustable reducer (0 to 400 rpm) moved a lever arm at a speed of 60 cycles/minute (1 Hz).
The implant/abutment assembly was connected to the lever arm, which performed a 10-mm linear course; this resulted in a linear speed of 20 mm/second. The antagonists were the flat, polished surfaces of five stainless steel cylinders. These cylinders were fixed in adjustable vertical loading poles. When the poles were released, their total weight (50 N) was transferred to the implant/abutment assemblies. Each simulated chewing cycle included three types of movement: a downward vertical movement (occlusion), a 10-mm
lateral movement (eccentric loading), and an upward vertical movement (disclusion). Each complete cycle was performed in 1 second, resulting in 60 cycles per minute (1 Hz), similar to the average human masticatory pace. 35–37 During occlusion and lateral movements,the total 50-N load was applied to the assemblies.
During disclusion, the assemblies were completely unloaded. Five assemblies were tested simultaneously. During the tests, the assemblies and the antagonist surfaces were completely immersed in deionized water. This mechanical loading device was designed according to International Organization for Standardization (ISO) norm 14569-2 under the Freiburg method. 38 Each mechanical loading test was carried out for 83.3 hours, for a total of 300,000 cycles for each assembly, which corresponded to approximately 1 year of normal masticatory function. 20,34,39.
After mechanical loading tests, assemblies were positioned in the torque measuring device, and loosening torque values were recorded (t1). Differences between tightening torque and loosening torque values for all assemblies were calculated, with loosening torque calculated as a percentage of the tightening torque. Relative values were calculated for the initial torque measurements (t0) and for the final torque measurements (t1) after mechanical loading.
Data were collected and an exploratory analysis was performed. Comparisons were made by orthogonal contrasts using the linear mixed effects model (random and fixed effects). This model is used in the analysis of data where the responses of the same specimen are grouped and an assumption of independence between observations in the same group is not suitable. The model fit was achieved using the PROCMIXED function of SAS 9.1 software (SAS Institute).
Results
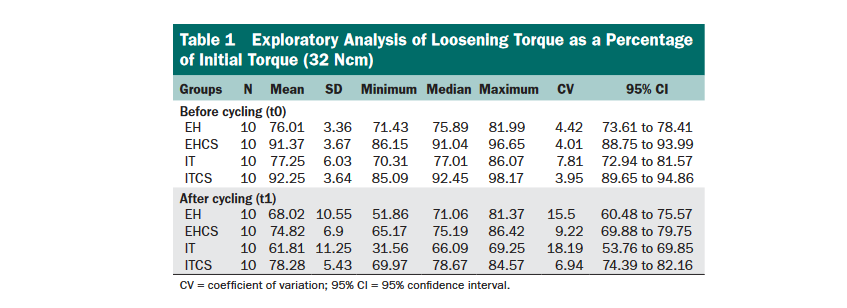
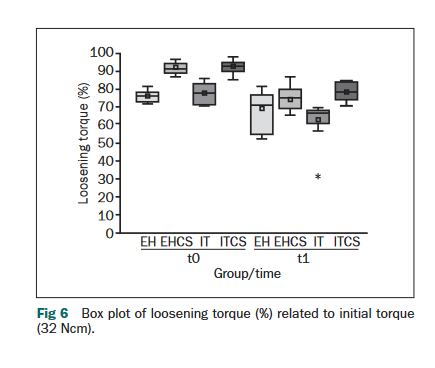
Table 1 and Fig 6 show the exploratory analysis of collected data. Comparisons among the experimental groups, before and after mechanical cycling, are shown in Table 2. Measurement of initial torque (t0) showed higher loosening torques for groups EHCS and ITCS than for groups EH and IT. EH and IT connections showed similar loosening torque values (Table 1). Final torque measurements (t1) after mechanical loading also showed higher loosening torques for groups EHCS and ITCS.
EH and IT connections again showed similar loosening torque values. After mechanical loading, a decrease in loosening torque values was seen for all groups. However, loosening torque values for the assemblies with experimental conical-head screws remained higher than for the assemblies with conventional flat-head screws after mechanical loading.
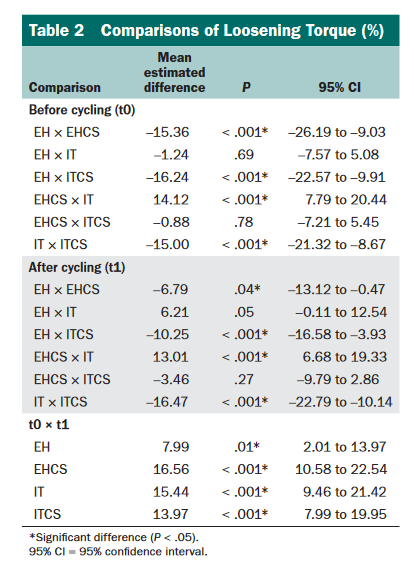
Statistical analysis (Table 2) revealed that, before mechanical cycling, there were significant differences between groups (P < .001), except for the comparisons EH × IT (P = .60) and for EHCS × ITCS (P = .78). After mechanical cycling, similarly, only the comparisons EH × IT (P = .05) and EHCS × ITCS (P = .27) showed no significant differences. Within the same groups, before and after mechanical cycling, all comparisons showed significant differences (P < .05).
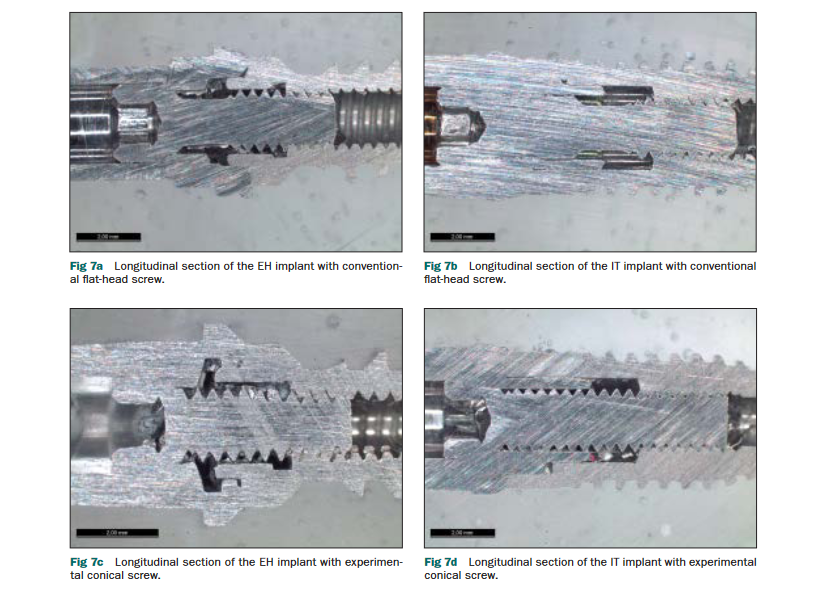
Optical microscopic analysis of the longitudinally sectioned implant/screw/abutment assemblies showed the differences between the profiles of the conventional and conical-head screws and the differences in their relationships with their respective abutments (Figs 7a to 7d). The conical screw showed increased contact between the conical head and the mating part of the abutment compared to the conventional flat-head screw, which showed no contact between the lateral portion of the head and the internal wall of the abutment.
The only active part of the flat-head screw was the bottom of the head, which was in contact with the mating part of the abutment; this area alone secured the entire assembly together. The conical-head screw presented a greater active surface area that clamped the assembly together (Figs 7c and 7d). disCussion Implant/abutment connection designs, such as EH or internal-hex with no frictional locking devices, have been associated with recurring mechanical problems.
The literature has highlighted screw loosening as the most frequent complication. 3–7,11,19,36,40 In vitro studies suggested superior mechanical behavior for connections with frictional locking components, compared to conventional screwed connections. 9,25,29,30,41–44 The results of the present study suggest that the use of conical-head abutment screws with frictional locking action resulted in greater connection stability and mechanical resistance compared to conventional flat-head screws, regardless of the connection design.
Long-term clinical studies are necessary to confirm the mechanical and biologic efficacy of various implant systems utilizing conical-head abutment screws. Coppedê et al 28 described a mechanical loading method similar to that employed in the present study. However, there were some limitations in that study, such as a loading force of 5 N anda limited loading period of 1,325 cycles, which corresponds to 3 to 4 days of oral function. For the present study, a novel mechanical loading machine was designed to simulate the dynamics of masticatory movement more precisely. The loading force was 50 N, which corresponds to normal chewing forces in the posterior region. 32,33,35,45 The literature is very controversial about this force value and cites values ranging from 17 N to as high as 3,500 N. 20,36,46–51 Conditions established in the new method resemble clinical masticatory conditions; each sample was cycled for 300,000 cycles, which corresponded to 1 year of normal oral function. 20,34,39,40,42,52,53 According to Winkler et al, 36 in vitro studies that examined screw loosening with hydraulic testing machines present considerable limitations because of the difficultiesin reproducing the complex nature of the masticatory cycle.
Thus, the improvements introduced in the present study were intended to provide results closer to those expected with clinical use of the components. In previous studies of the mechanical behavior of implant-supported prostheses, the only force value considered to examine the effects of occlusal loading was the masticatory force.32–34,36,47,49 However, masticatory force values alone are incomplete; the effects over the restorations depend on the relationship of the masticatory force with the effective occlusal area.
The relationship between masticatory force and effective occlusal area determines the tension that is generated over the restoration.48 The tension value is more relevant to the mechanical effects of the restorations than the masticatory force itself. The samples of the present study were subjected to high tension values. Considering the masticatory force used (50 N) and the effective occlusal surface area of the abutments (7.06 mm2), the tension value obtained was 7.08 N/mm2, which is comparable to the high occlusal tensions generated in posterior areas.48 Lateral movements in the chewing cycles in the present study subjected the assemblies to high eccentric forces, which are less favorable than axial forces.2 In vivo studies have reported mean lateral loads of 25 N on implant-supported prostheses during masticatory function.54 In the present study, lateral movements were executed with a 50-N load applied over the samples in a 10-mm linear course. This generated considerable eccentric loading and vibration as a result of the friction between thabutment’s occlusal surface and the stainless steel antagonist surface.
These loads subjected the abutment screws to high stresses. These loading conditions possibly created in vitro conditions thawere more demanding than normal conditions in vivo. In vivo analyses are necessary to confirm these results.
Cantwell and Hobkirk55 emphasized the influence of screw head shape on the amount of preload obtained. The present study proposed a new screw head shape intended to improve the implant/abutment screw joint. These conical-head screws incorporated a 25-degree taper in its head, which created a friction-locking mechanism. Therefore, in addition to the locking provided by the threads of the screw, an additional friction-locking effect occurred between the screw head and the mating internal parts of the abutment, which resisted rotational micromovements of the screw and thereby reduced torque loss.
Thus, a more effective protection of screw preload occurred during mechanical loading. The results of this in vitro investigation suggest that there was a significant difference (P = .000) inthe residual preload between the two types of screws. Conical-head screws presented loosening torques that were significantly higher than those of conventional flat-head screws. Clinically, these findings could translate into more stable screw connections, regardless of the implant system. The improved stability could be relevant in highly demanding situations, such as single-tooth restorations, restorations in the posterior area, or cemented restorations, which present less reversibility.
In these situations there would be a reduced possibility of screw loosening. The different macrogeometries (conical and cylindric) and the different connection types (EH or IT) of the implants used in this study could have significant effects on the load transfer to the screws. The division of the assemblies into four different groups was meant to allow the separate identification of the effects of the implant form on the loosening of the screws. Comparisons within the groups with the same type of screw revealed that the form of the implant presented no significant influence on the loosening torque of theabutment screws.
The results of the present study are in contrast with previous papers,56,57 which stated that higher preload values for a determined amount of torque were obtained with flat-head screws compared to conical-head or beveled-head screws. Engineering problems may explain the poor results obtained in these earlier investigations of conical-head screws. Slight modifications in the design of the taper can dramatically alter the results obtained with conical-head screws. The exact amount of taper and the ideal length of the tapered section of the abutment screw head remain to be determined.
However, the design proposed in this study presented promising results. These results should be confirmed by other in vitro studies. Mechanically and structurally ideal characteristics of the experimental conical-head screws should be determined in specific tests and validated by clinical studies. Moreover, structural and surface enhancements may improve the results obtained in thepresent study. New investigations should be conducted to develop all possible improvements to obtain screws that provide high long-term stability.
ConClusions
Within the limitations of this in vitro study, the following conclusions were drawn:
1. Experimental conical-head abutment screws presented higher loosening torque values compared to conventional flat-head screws before and after mechanical cyclic loading equivalent to 1 year of oral function.
2. The design of the implant/abutment connection presented no significant influence on the loosening torque of the abutment screws.
aCKnowledGMents
The authors would like to acknowledge Dérig Industry and Commerce of Tools Ltd. (São Paulo, Brazil) for producing and providing the experimental implants, screws, and components used in this investigation. The authors disclose no other financial or personal relationships that could inappropriately influence or bias this work.
ReFerenCes
1. Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg 1977;suppl 16:1–132.
2. Rangert B, Jemt T, Jörneus L. Forces and moments on Brånemark implants. Int J Oral Maxillofac Implants 1989;4:241–247.
3. Jemt T, Lekholm U, Gröndahl K. A 3-year followup study of early single implant restorations ad modum Brånemark. Int J Periodontics Restorative Dent 1990;10:340–349.
4. Jemt T, Laney W, Harris D, et al. Osseointegrated implants for single tooth replacement: A 1-year report from a multicenter prospective study. Int J Oral Maxillofac Implants 1991;6:29–36.
5. Becker W, Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: A retrospective study. J Prosthet Dent 1995;74:51–55.
6. Wie H. Registration of localization, occlusion and occluding materials for failing screw joints in the Brånemark implant system. Clin Oral Implants Res 1995;6:47–53.
7. Balshi TJ, Hernandez RE, Pryszlak MC, Rangert B. A comparative study of one implant versus two replacing a single molar. Int J Oral Maxillofac Implants 1996;11:372–378.
8. Laney WR, Jemt T, Harris D, et al. Osseointegrated implants for single-tooth replacement: Progress report from a multicenter prospective study after 3 years. Int J Oral Maxillofac Implants 1994;9:49–54.
9. Norton MR. An in vitro evaluation of the strength of an internal conical interface compared to a butt joint interface in implant design. Clin Oral Implants Res 1997;8:290–298.
10. Levine RA, Clem DS III, Wilson TG Jr, Higginbotton F, Solnit G. Multicenter retrospective analysis of the ITI implant system used for single tooth replacements: Results of loading for 2 or more years. Int J Oral Maxillofac Implants 1999;14:516–520.11. Burguete RL, Johns RB, King T, Patterson EA. Tightening characteristics for screwed joints in osseointegrated dental implants. J Prosthet Dent 1994;71:592–599.
12. Norton MR. Assessment of cold welding properties of the internal conical interface of two commercially available implant systems. J Prosthet Dent 1999;81:159–166.
13. Martin WC, Woody RD, Miller BH, Miller AW. Implant abutment screw rotations and preloads for four different screw materials and surfaces. J Prosthet Dent 2001;86:24–32.
14. Mitrani R, Nicholls JI, Phillips KM, Ma T. Accuracy of electronic implant torque controllers following time in clinical service. Int J Oral Maxillofac Implants 2001;16:394–399.
15. Standlee JP, Caputo AA, Chwu MJ, Sun TT. Accuracy of mechanical torque-limiting devices for implants. Int J Oral Maxillofac Implants 2002;17:220–224.
16. Tan KB, Nicholls JI. The effect of 3 torque delivery systems on gold screw preload at the gold cylinder-abutment screw joint. Int J Oral Maxillofac Implants 2002;17:175–183.
17. Drago CJ. A clinical study of the efficacy of Gold-Tite square abutment screws in cemented-retained implant restorations. Int J Oral Maxillofac Implants 2003;18:273–278.
18. Çehreli MC, Akça K, Iplikçioglu H. Force transmission of one- and two-piece morse-taper oral implants: A nonlinear finite element analysis. Clin Oral Implants Res 2004;15:481– 89.
19. Cho SC, Small PN, Elian N, Tarnow D. Screw loosening for standard and wide diameter implants in partially edentulous cases: 3- to 7-year longitudinal data. Implant Dent 2004;13:245–250.
20. Khraisat A, Hashimoto A, Nomura S, Miyakawa O. Effect of lateral cyclic loading on abutment screw loosening of an external hexagon implant system. J Prosthet Dent 2004;91:326–324.
21. Preiskel HW, Tsolka P. Cement- and screw-retained implant-supported prostheses: Up to 10 years of follow-up of a new design. Int J Oral Maxillofac Implants 2004;19:87–91.
22. Nedir R, Bischof M, Szmukler-Moncler S, Belser UC, Samson J. Prosthetic complications with dental implants: From an up-to-8- year experience in private practice. Int J Oral Maxillofac Implants 2006;21:919–928.
23. Hill EE, Phillips SM, Breeding LC. Implant abutment screw torque generated by general dentists using a hand driver in a limited access space simulating the mouth. J Oral Implantol 2007;33:277–279.
24. Stüker RA, Teixeira ER, Beck JCP, Costa NP. Preload and torque removal evaluation of three different abutment screws for single standing implant restorations. J Appl Oral Sci 2008;16:55–58.
25. Theoharidou A, Petridis HP, Tzannas K, Garefis P. Abutment screw loosening in single-implant restorations: A systematic review. Int J Oral Maxillofac Implants 2008;23:681–690.
26. Vallee MC, Conrad HJ, Basu S, Seong WJ. Accuracy of friction-style and spring-style mechanical torque limiting devices for dental implants. J Prosthet Dent 2008;100:86–92.
27. Dailey B, Jordan L, Blind O, Tavernier B. Axial displacement of abutments into implants and implant replicas, with the tapered conescrew internal connection, as a function of the tightening torque. Int J Oral Maxillofac Implants 2009;24:251–256.
28. Coppedê AR, Mattos MGC, Rodrigues RCS, Ribeiro RF. Effect of repeated torque/mechanical loading cycles on two different abutment types with internal tapered connections: An in vitro study. Clin Oral Implants Res 2009;20:624–632.
29. Merz BR, Hunenbart S, Belser UC. Mechanics of the implantabutment connection: An 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants 2000;15:519–526.
30. Coppedê AR, Bersani E, Mattos MGC, Rodrigues RCS, Sartori IAM, Ribeiro RF Fracture resistance of the implant-abutment connection in implants with internal hex and internal conical connections under oblique compressive loading: An in vitro study. Int J Prosthodont 2009;22:283–286.
31. Kitagawa T, Tanimoto Y, Odaki M, Nemoto K, Aida M. Influence of implant/abutment joint designs on abutment screw loosening in a dentaimplant system. J Biomed Mater Res B Appl Biomater 2005;75:457–463.
32. Hobkirk JA, Psarros KJ. The influence of occlusal surface material on peak masticatory forces using osseointegrated implant-supported prostheses. Int J Oral Maxillofac Implants 1992;7:345–352.
33. Richter EJ. In vivo vertical forces on implants. Int J Oral Maxillofac Implants 1995;10:99–108.
34. Gateau P, Sabek M, Dailey B. Fatigue testing and microscopic evaluation of post and core restorations under artificial crowns. J Prosthet Dent 1999;82:341–347.
35. Attia A, Kern M. Influence of cyclic loading and luting agents on the fracture load of two all-ceramic crown systems. J Prosthet Dent 2004;92:551–556.
36. Winkler S, Ring K, Ring JD, Boberick KG. Implant screw mechanics and the settling effect: An overview. J Oral Implantol 2003;29:242–245.
37. Kim SG, Park JU, Jeong JH, Bae C, Bae TS, Chee W. In vitro evaluation of reverse torque value of abutment screw and marginal opening in a screw- and cemented-retained implant fixed partial denture design. Int J Oral Maxillofac Implants 2009;24:1061–1067.
38. ISO norm ISO/TS 14569-2:2001. Dental Materials – Guidance on testing of wear – Part 2: Wear by two – and/or three body contact. Geneva, Switzerland: ISO, 2001.
39. Quek CE, Tan KB, Nicholls JI. Load fatigue performance of a single-tooth implant abutment system: Effect of diameter. Int J Oral Maxillofac Implants 2006;21:929–936.
40. Tsuge T, Hagiwara Y. Influence of lateral-oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent Mater J 2009;28:373–381.
41. Sutter F, Weber HP, Sorensen J, Belser U. The new restorative concept of the ITI dental implant system: Design and engineering. Int J Periodontics Restorative Dent 1993;13:409– 31.
42. Khraisat A, Stegaroiu R, Nomura S, Miyakawa O. Fatigue resistance of two implant/abutment joint designs. J Prosthet Dent 2002;88: 604–610.
43. Akça K, Çehreli MC, Iplikçioglu H. Evaluation of the mechanical characteristics of the implant-abutment complex of a reduced diameter morse-taper implant. A nonlinear finite element stress analysis. Clin Oral Implants Res 2003;14:444–454.
44. Park JK, Choi JU, Jeon YC, Choi KS, Jeong CM. Effects of abutment screw coating on implant preload. J Prosthodont 2010;19:458–464.
45. Khraisat A, Baqain ZH, Smaadi L, Nomura S, Miyakawa O, Elnasser Z. Abutment rotational displacement of external hexagon implant system under lateral cyclic loading. Clin Implant Dent Relat Res 2006;8:96–99.
46. Binon PP. The effect of implant/abutment hexagonal misfit on screw joint stability. Int J Prosthodont 1996;9:149–160.
47. Tortopidis D, Lyons MF, Baxendale RH, Gilmour WH. The variability of bite force measurement between sessions, in different positions within the dental arch. J Oral Rehabil 1998;25:681–686.
48. Hidaka O, Iwasaki M, Saito M, Morimoto T. Influence of clenching intensity on bite force balance, occlusal contact area, and average bite pressure. J Dent Res 1999;78:1336–1344.
49. Morneburg TR, Proschel PA, Nat R. Measurement of masticatory forces and implant loads: A methodologic clinical study. Int J Prosthodont 2002;15:20–27.
50. Curtis AR, Wright AJ, Fleming GJP. The influence of simulated masticatory loading regimes on the bi-axial flexure strength and reliability of a Y-TZP dental ceramic. J Dent 2006;34:317–325.
51. Oie E, Horiuchi M, Soma K. Effects of occlusal contact and its area on gravity fluctuation. Angle Orthod 2010;80:540–546.
52. Breeding LC, Dixon DL, Nelson EW, Tietge JD. Torque required to loosen single-tooth implant abutment screws before and after simulated function. Int J Prosthodont 1993;6:435– 39.
53. Dixon DL, Breeding LC, Sadler JP, McKay ML. Comparison of screw loosening, rotation and deflection among three implant designs. J Prosthet Dent 1995;74:270–278.
54. Morneburg TR, Proschel PA. In vivo forces on implants influenced by occlusal scheme and food consistency. Int J Prosthodont 2003;16: 481–486.
55. Cantwell A, Hobkirk JA. Preload loss in gold prosthesis-retaining screws as function of time. Int J Oral Maxillofac Implants 2004;19: 124–132.
56. Jörnéus L, Jemt T, Carlsson L. Loads and designs of screw joints for single crowns supported by osseointegrated implants. Int J Oral Maxillofac Implants 1992;7:353–359.
57. Piermatti J, Yousef H, Luke A, Mahevich R, Weiner S. An in vitro analysis of implant screw torque loss with external hex and internal connection implant systems. Implant Dent 2006;15:427–435.
