The purpose of this study was to present a protocol for the replacement of single teeth lost in the molar area with immediate implantation in fresh extraction sockets, no flap reflections or grafting procedures, and immediate loading. Twentythree implants were placed in 20 patients between 2000 and 2006. No implants were lost and no signs of significant bone resorption, loss of osseointegration, or soft tissue complications were reported. The results of this study indicate that this protocol may be a feasible alternative for the replacement of condemned molars. (Int J Periodontics Restorative Dent 2010;30:291–299.)
*Private Practice in Implantology and Oral Rehabilitation, Ribeirao Preto, São Paulo, Brazil.
**Private Practice in Implantology and Oral Rehabilitation, Belo Horizonte, Minas Gerais, Brazil.
Correspondence to: Dr Edmilson Bersani, Rua Joaquim de Abreu Machado, 142,
Ribeirania, Ribeirao Preto, SP, Brazil CEP 14.096–139; fax: 55 (16) 3618 4481;
email: bersanied@terra.com.br.
In the early days of implant dentistry, a two-stage surgery was believed mandatory to provide a submerged, stress-free healing period for the implants to osseointegrate.1,2 In cases of tooth extraction, complete healing of the alveolar bone was required before placing an implant, according to Brånemark’s original principles. 2 This process required 6 to 12 months, and during this period, a considerable amount of bone can be lost as a result of bone resorption.3,4 In the past decades, implant dentistry has undergone a series of advances that allowed for modification of the original protocol. Single-tooth
replacement became a predictable treatment option,5–7 even in the posterior regions of the mandible and maxilla. 8,9 Immediate and early loading protocols have shown similar success rates to the conventional delayed protocol. 10–12
Atraumatic extraction techniques were developed to minimize surgical trauma to the alveolar bone.6,13 Flapless surgeries have become a reality, when the indications for its use are clear.14–16 Immediate placement of implants in fresh extraction sockets has been demonstrated also to be a successful procedure that helps in preventing bone resorption.17–20 Grafting procedures have been proposed as a means to enhance bone formation around implants placed in fresh extraction sockets with good results.18,21–24 Graftless procedures have also resulted in good outcomes in the anterior and premolar areas.3,7,13,25–27 Studies that performed graftless procedures in the molar area showed some areas of incomplete bone healing.17,26,28–31 No studies were found on the immediate loading of implants placed in fresh extraction sockets in the molar area.
Therefore, the aim of this study was to present a were immediately loaded in fresh extraction sockets of molars with a flapless approach and without the use of grafting procedures. Method and materials Study population The study population consisted of 20 patients (9 men, 11 women), with ages ranging from 24 to 68 years (mean age, 50.5 years), who presented for extraction of a single molar and replacement with an implant-supported prosthesis in a private practice in Ribeirao Preto, São Paulo, Brazil.
Surgical and prosthetic procedures were performed by two experienced surgeons. Indications for tooth extraction were related to: longitudinal tooth fracture (10 cases), untreatable caries (2 cases), periodontal disease (8 cases), endodontic treatment failure (2 cases), and root perforation (1 case). Inclusion criteria were as follows: a need for single molar extraction and immediate placement of an implant, stable and functional occlusion with no signs or symptoms of occlusal pathologies or articular disorders, ability and willingness of the patient to follow the study protocol, and good overall health and oral hygiene.
Bone volume at the extraction site was assessed by means of periodontal probing and radiographic measurements. A minimum mesiodistal and buccolingual length of 7 mm and a minimum height of 11 mm from the cervical limit of the buccal wall to the anatomical limits (maxillary sinus and mandibular canal) were required to allow the placement of implants with a minimum diameter of 4.5 mm and a minimum length of 10 mm. A minimum bone length of 3 mm from the apical portion of the socket to the anatomical limits was also required to achieve extra anchorage in the apical portion of the implant.
Patients who did not present with these bone dimensions were excluded. In addition to the aforementioned, exclusion criteria included compromised general health, conditions that could lead to osseointegration problems, parafunctional habits such as bruxism, poor oral hygiene, and malocclusions that could lead to occlusal interferences in the posterior teeth during eccentric movements. The integrity of the buccal bone wall was clinically assessed by means of periodontal probing and analysis of periapical radiographs.
When a partial buccal bone wall loss was detected, the patient was excluded from the study. Smoking was not an exclusion criterion. Among the 20 patients treated in this study, 3 were smokers (15%). Diagnosis and treatment planning included: study models articulated in a semiadjustable articulator, a diagnostic wax-up, a surgical guide, a provisional acrylic resin crown, clinical photographs, and periapical and panoramic radiographs. All possible treatment options were offered to the patients. Patients enrolled in the study authorized the procedure by signing a consent form according to the Helsinki Declaration.
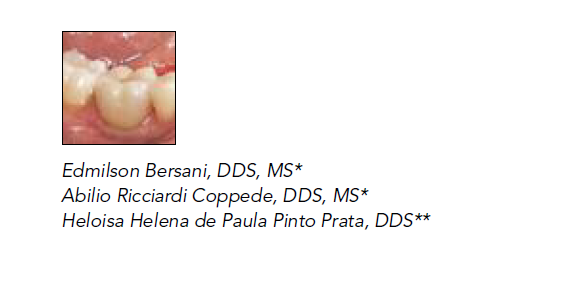
Surgical guide preparation
Implant positioning in a flapless surgery is critical. For this reason, acrylic resin surgical guides were prepared prior to the surgeries (Fig 1). The remaining coronal portions of the molars were cut off and the surgical guides were installed for radiographic evaluation (Fig 2). The surgical guides oriented the initial osteotomies, creating a path for the subsequent surgical drills at the correct angulation.
Surgical protocol
All patients were given prophylactic treatment 1 hour before surgery that included 1.5 g amoxicilin and potassium clavulanate, 4 mg dexamethasone, and 750 mg paracetamol. Local anesthesia was performed at all extraction sites. The teeth were extracted using an atraumatic technique. No incisions or flaps were made. The roots were separated using diamond burs and gently lifted using periotomes.
The socket was degranulated with surgical curettes and carbide burs and irrigated abundantly with sterile saline. The surgical guide was then placed in position and the initial osteotomy was performed. The complete osteotomy was obtained after using all surgical drills. The implants used in this study included: Replace Select Tapered (Nobel Biocare), Alvim II Internal Hex (Neodent Implante Osseointegrável), and Alvim CM Morse Taper (Neodent Implante Osseointegrável).
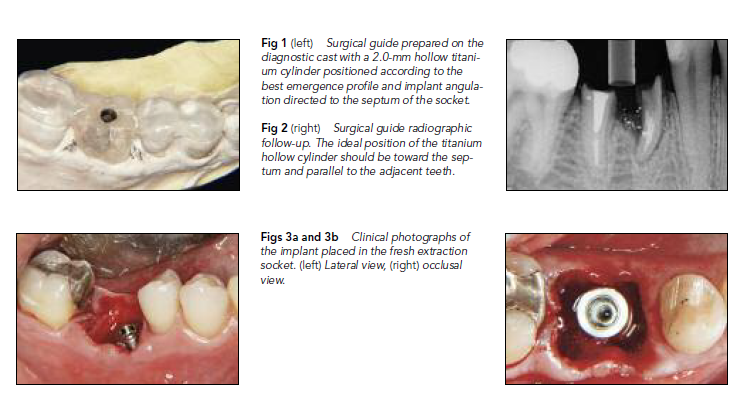
The implants were placed with a mandatory insertion torque of at least 35 Ncm (Figs 3a and 3b).17 The maximum insertion torque allowed was 50 Ncm to avoid overcompression of the surrounding bone. Torque was measured by a drill unit (SI-95 115, W & H Implant Med). Sites in which the insertion torque did not reach 35 Ncm were excluded from the study.
Prosthetic protocol
After implant placement, a provisional acrylic resin crown was adapted to the temporary abutment chairside. The provisional abutments used in this study were machined metallic abutments. Both screwed and cemented provisional crowns were used in this study. Replace Select Tapered and Alvim II Internal Hex implants received screwed provisional crowns, and Alvim CM Morse Taper implants received cemented provisional crowns with a temporary cement (Rely X Temp, 3M ESPE), amounting to a total of 14 screwed and 9 cemented provisional crowns.
The emergence profiles of the crowns were adjusted to guide soft tissue healing. The natural anatomy of the sockets and soft tissues was not affected by the atraumatic surgeries so the contours of the crowns were adjusted to match the gingival contour perfectly. Suture procedures were not mandatory and were performed only in cases where the socket dimensions were wider than the optimal profile of the provisional crown, providing a better relationship between the soft tissues and the provisional restoration (Fig 4).
Interrupted sutures with mononylon 5.0 and 6.0 threads (Ethicon, Johnson & Johnson) were used. Occlusal adjustments of the provisional crowns wer conducted clinically using an interocclusal carbon articulating paper (AccuFilm II). Functional occlusal contacts were preserved in the provisional crowns. No contacts were allowed during eccentric movements. Adjustments were made with fine-grit diamond burs. The definitive crowns were inserted according to patient convenience after a minimum healing period of 4 months. The principles of occlusion used for the definitive crowns followed the same principles used for the provisionals.All definitive restorations were ceramic crowns; 14 were screwed and 9 were cemented. For the cemented crowns, zinc cement (Fleck’s, Mizzy) was used as the luting agent.
Clinical and radiographic evaluation
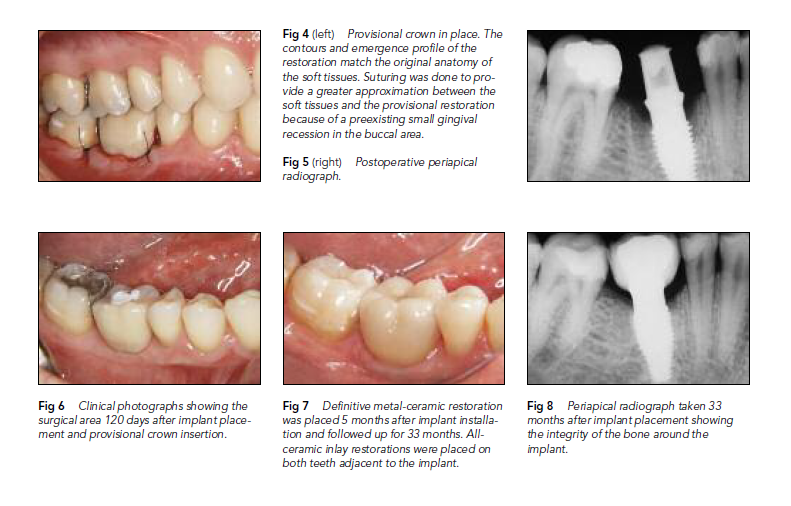
Periapical radiographs were taken immediately after implant placement and placement of the provisional crown to evaluate the fit of the abutment and the crestal bone levels at baseline (Fig 5). The standard procedure included the use of an x-ray positioning device and the parallelism technique. Subsequent evaluations took place at 30, 60, 120, and 360 days after implant placement. At follow-up appointments, patients underwent periodontal probing and had periapical radiographs taken. After that, follow-up continued on a yearly basis (Figs 6 to 8).
Results
In this study, 23 implants were placed in 20 patients from 2000 to 2006. All patients were followed up with at implant placement, during the provisional period, and after insertion of the definitive restoration. The minimum period of follow-up was 4 months and (evidenced by radiographic evaluation), as suggested by Misch. 32Clinical conditions were assessed at all followup appointments; patients were examined by means of periodontal probing, radiographs, and intraoral photographs. All implants were stable and with no signs of infection, inflammation, bleeding, or loss of osseointegration. the maximum was 85 months.
All patients had an undisturbed healing period. No implants failed throughout the follow-up period. The success criteria used in this study were absence of pain, stability of the implant, probing depth, bone resorption, presence of bleeding, and the absence of any radiopaque areas around the implant
Discussion
The initial stages of healing after tooth extraction are critical to the bone resorption26 that occurs indefinitely and progressively during the first year, during which up to 44% of the alveolar ridge can be lost.3,4,7,19,20 Immediate implantation is an important aspect in preventing local bone resorption after tooth extraction.17,19,25 In extraction sites, a main concern is the thickness of the buccal wall of the socket. After tooth extraction, the remaining buccal wall is usually very thin and should be preserved carefully.
The periodontal attachment and the buccal mucosa are the main sources of blood to the buccal bone wall. When a tooth is removed, the periodontal attachment is also taken away, so if a buccal flap is reflected, the blood supply to the local bone will be severely compromised, leading to a greater chance of local resorption.33,34 Performing a flapless surgery in a fresh extraction site is meant to minimize the resorption of the buccal wall, ultimately preventing the occurrence of buccal dehiscences.
In this study, all surgeries were flapless to maintain local tissue architecture, and the provisional restoration acted like a frame, following the original contour, to guide gingival healing.6,13,15 Grafting materials and guided regeneration techniques have been used to prevent fibrous tissue formation around the implant and to maximize the bone-implant contact surface when implants are placed in fresh extraction sockets.6,21–24 Human and animal studies regarding the concept of “jumping distance,” which is the distance between the implant and the internal walls of the socket, agree that gaps smaller than 1.5 to 2 mm will heal predictably if no filling materials or barrier membranes are used.3,7,13,25,35.
The outcomes published for graftless procedures in molar areas, where the defects are almost always larger than 2 mm, show the occurrence of some areas of incomplete bone healing. 17,26,28–31 These studies were conducted with primary wound closure models in which the implants were not immediately loaded. In this study, no grafting materials or barrier membranes were used, and all implants were osseointegrated during the follow-up period. By means of periodontal probing and radiographic images, the presence of hard tissue around the crestal area of the implants was verified.
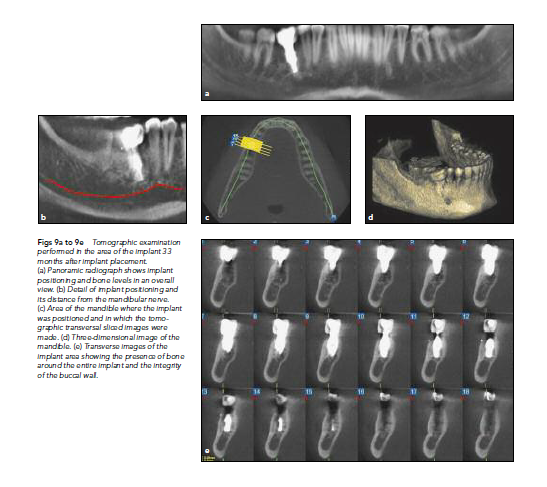
Computed tomography scans were performed after complete bone healing and showed significant bone width around the implants (Figs 9a to 9e). These findings can be associated with the closure of the socket by the customized provisional crown, which acted like a customized healing abutment. This provisional crown has a similar effect to a nonreabsorbable membrane that tolerates the presence of plaque and maintains the closure of the socket, even when exposed to the oral environment.
In addition, the functional stimulation determined by the immediate loading of the implant may influence bone remodeling around the implant, providing a greater boneimplant contact compared to the primary wound closure models available in the literature.36 Histomorphometric evaluations of implants inserted according to this technique must be performed in future studies to confirm these clinical findings.
The inclusion and exclusion criteria must be followed meticulously to increase the predictability of this protocol. Single cases with complete or partial lack of the buccal wall in molar extraction sites, chronic lesions capable of altering the socket topography, or cases in which the implants did not reach the minimum insertion torque of 35 Ncm were not treated according to the described technique. In this study, there were no implant failures reported.
The limited number of implants included in the study is not enough to draw any definitive conclusions regarding the success of this therapeutic protocol, although it seems to be promising. Further studies are needed to confirm its efficiency and to establish a more precise success rate.
Conclusions
The findings of this case series suggest that the immediate loading of implants placed in fresh extraction sockets in the molar area with no grafting procedures is a predictable method to replace single lost molars—if the inclusion and exclusion criteria and the described technique are followed meticulously. Despite the fact that the number of cases presented in this paper is not sufficient to draw any definitive conclusions, the results obtained suggest that this protocol may be the treatment of choice for replacing single molars that fulfill all prerequisites. These clinical findings must be confirmed by prospective, randomized controlled clinical trials with careful experimental design before thi protocol can be recommended for general use.
References
- Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl 1977;16:1–132.
- Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981;10:387–416.
- Paolantonio M, Dolci M, Scarano A, et al. Immediate implantation in fresh extraction sockets. A controlled clinical and histological study in man. J Periodontol 2001; 72:1560–1571.
- Carlsson GE, Persson G. Morphologic changes of the mandible after extraction and wearing dentures. A longitudinal, clinical, and x-ray cephalometric study covering 5 years. Odontol Revy 1967;18:27–54.
- Kemppainen P, Eskola S, Ylipaavalniemi P. A comparative prospective clinical study of two single-tooth implants: A preliminary report of 102 implants. J Prosthet Dent 1997;77:382–387.
- Tepret F, Sertgöz A, Basa S. Immediately loaded anterior single-tooth implants: Two cases. Implant Dent 2005;14:242–247. Barone A, Rispoli L, Vozza I, Quaranta A, Covani U. Immediate restoration of single implants placed immediately after tooth extraction. J Periodontol 2006;77: 1914–1920.
- Balshi TJ, Hernandez RE, Pryszlak MC, Rangert B. A comparative study of one implant versus two replacing a single molar. Int J Oral Maxillofac Implants 1996; 11:372–378.
- Henry PJ, Laney WR, Jemt T, et al. Osseo – integrated implants for single-tooth replacement: A prospective 5-year multicenter study. Int J Oral Maxillofac Implants 1996;11:450–455.
- Schnitman PA, Wöhrle PS, Rubenstein JE, DaSilva JD, Wang NH. Ten-year results for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxollofac Implants 1997;12:495–503.
- Ericsson I, Nilson H, Lindh T, Nilner K, Randow K. Immediate functional loading of Brånemark single tooth implants. An 18 months’ clinical pilot follow-up study. Clin Oral Implants Res 2000;11:26–33.
- Testori T, Meltzer A, Del Fabbro M, et al. Immediate occlusal loading of Osseotite implants in the lower edentulous jaw. A multicenter prospective study. Clin Oral Implants Res 2004;15:278–284.
- Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1- year prospective study. Int J Oral Maxillofac Implants 2003;18:31–39.
- Becker W, Wikesjö UM, Sennerby L, et al. Histologic evaluation of implants following flapless and flapped surgery: A study in canines. J Periodontol 2006;77:1717–1722.
- Oh TJ, Shotwell JL, Billy EJ, Wang HL. Effect of flapless implant surgery on soft tissue profile: A randomized controlled clinical trial. J Periodontol 2006;77:874–882.
- Campelo LD, Camara JR. Flapless implant surgery: A 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants 2002;17:271–276.
- Schropp L, Kostopoulos L, Wenzel A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets: A prospective clinical study. Int J Oral Maxillofac Implants 2003;18:189–199.
- Nemcovsky CE, Artzi Z, Moses O, Gelernter I. Healing of marginal defects at implants placed in fresh extraction sockets or after 4-6 weeks of healing. A comparative study. Clin Oral Implants Res 2002;13: 410–419.Denissen HW, Kalk W, Veldhuis AH, van Waas MAJ. Anatomic consideration for preventive implantation. Int J Oral Maxillofac Implants 1993;8:191– 96.
- Watzek G, Haider R, Mensdorff-Pouilly N, Haas R. Immediate and delayed implantation for complete restoration of the jaw following extraction of all residual teeth: A retrospective study comparing different types of serial immediate implantation. Int J Oral Maxillofac Implants 1995;10:561–567.
- Fugazzotto PA. Implant placement at the time of maxillary molar extraction: Technique and report of preliminary results of 83 sites. J Periodontol 2006;77:302–309.
- Prosper L, Gherlone EF, Redaelli S, Quaranta M. Four-year follow-up of largerdiameter implants placed in fresh extraction sockets using a resorbable membrane or a resorbable alloplastic material. Int J Oral Maxillofac Implants 2003;18:856–864.
- Schliephake H, Kracht D. Vertical ridge augmentation using polylactic membranes in conjunction with immediate implants in periodontallycompromised extraction sites: An experimental study in dogs. Int J Oral Maxillofac Implants 1997;12:325–334.
- Scarano A, Iezzi G, Petrone G, Marinho VC, Corigliano M, Piattelli A. Immediate postextraction implants: A histologic and histometric analysis in monkeys. J Oral Implantol 2000;26:163–169.
- Covani U, Cornelini R, Barone A. Bucco-lingual bone remodeling around implants placed into immediate extraction sockets: A case series. J Periodontol 2003;74: 268–273.
- Covani U, Bortolaia C, Barone A, Sbordone L. Bucco-lingual crestal bone changes after immediate and delayed implant placement. J Periodontol 2004;75:1605–1612.
- Becker W, Sennerby L, Bedrossian E, Becker BE, Lucchini JP. Implant stability measurements for implants placed at the time of extraction: A cohort, prospective clinical trial. J Periodontol 2005;76:391–397.
- Wilson TG Jr, Schenk R, Buser D, Cochran D. Implants placed in immediate extraction sites: A report of histologic and histometric analyses of human biopsies. Int J Oral Maxillofac Implants 1998;13:333–341.
- Botticelli D, Berglundh T, Lindhe J. Hardtissue alterations following immediate implant placement in extraction sites. J Clin Periodontol 2004;31:820– 28.
- Botticelli D, Berglundh T, Buser D, Lindhe J. Appositional bone formation in marginal defects at implants. Clin Oral Implants Res 2003;14:1–9.
- Jung UW, Kim CS, Choi SH, Cho KS, Inoue T, Kim CK. Healing of surgically created circumferential gap around non-submergedtype implants in dogs: A histomorphometric study. Clin Oral Implants Res 2007;18: 171–178.
- Misch CE. Contemporary Implant Dentistry. St Louis: Mosby, 1993:779.
- Kan JY, Rungcharassaeng K, Ojano M, Goodacre CJ. Flapless anterior implant surgery: A surgical and prosthodontic rationale. Pract Periodontics Aesthet Dent 2000;12:467–474.
- Petrungaro PS. Immediate restoration of implants utilizing a flapless approach to preserve interdental tissue contours. Pract Proced Aesthet Dent 2005;17:151–158.
- Barzilay I, Graser GN, Iranpour B, Natiella JR, Proskin HM. Immediate implantation of pure titanium implants into extraction sockets of Macaca fascicularis. Part II: Histologic observations. Int J Oral Maxillofac Implants 1996;11:489–497.
- Skalak R. A brief essay on the philosophy of a one-step versus a two-step procedure for osseointegrated fixture-supported dental prostheses. In: Brånemark PI. The Brånemark Novum Protocol for Same-day Teeth: A Global Perspective. Berlin: Quintessenz, 2001:16–20.
Copyright of International Journal of Periodontics & Restorative Dentistry is the property of Quintessence Publishing Company Inc. and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder’s express written permission. However, users may print, download, or email articles for individual use.
