Fracture Resistance of the Implant-Abutment Connection in Implants with Internal Hex and Internal Conical Connections Under Oblique Compressive Loading: An In Vitro Study
Abílio Ricciardi Coppedê, DDS, MSca/Edmilson Bersani, DDS, MSca/Maria da Gloria Chiarello de Mattos, DDS, MSc, PhDb/Renata Cristina Silveira Rodrigues, DDS, MSc, PhDc/Ivete Aparecida de Mattias Sartori, DDS, MSc, PhDd/Ricardo Faria Ribeiro, DDS, MSc, PhDb
The objective of this study was to verify if differences in the design of internal hex (IH) and internal conical (IC) connection implant systems influence fracture resistance under oblique compressive forces. Twenty implant-abutment assemblies were utilized: 10 with IH connections and 10 with IC connections. Maximum deformation force for IC implants (90.58 ± 6.72 kgf) was statistically higher than that for IH implants (83.73 ± 4.94 kgf) (P = .0182). Fracture force for the IH implants was 79.86 ± 4.77 kgf. None of the IC implants fractured. The friction-locking mechanics and the solid design of the IC abutments provided greater resistance to deformation and fracture under oblique compressive loading when compared to the IH abutments. Int J Prosthodont 2009;22:283–286.
Internal hex connections were designed to increase the implant-abutment contact surface area in order to improve abutment stability. It has been shown that internal hex implants provide better force distribution when compared with external hex implants.1 However, there is no frictional locking between the mating parts of the abutment and the implant and most of these forces are resisted by the screw preload.1 If the preload is exceeded, the screw is prone to loosening or fracture. Internal conical connections provide an intimate implant-abutment contact, which is meant to improve the mechanical stability of the abutment and avoid abutment loosening. 2 The fixation and stability of these systems are not functions of the screw; they are granted by the frictional resistance resulting from the contact between the conical mating parts of the abutment and the implant. 2 The good stability obtained by this system seems to provide a high resistance to bending forces at the implant-abutment interface.
3 The objective of this study was to determine if the dif-ferent design, dimensions, and mechanical properties of the abutments and implant-abutment connections of internal hex and internal conical connection systems influence fracture resistance under oblique compres-sive loads.
Materials and Methods
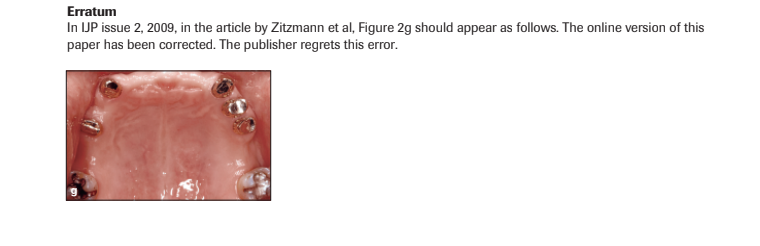
This study used two implant systems: Alvim II Plus (Neo-dent Implante Osseointegrável) with a 1.5-mm-high in-ternal hex (IH) connection and Alvim CM (Neodent Implante Osseointegrável) with an 11.5-degree, 3.5-mm-high internal conical (IC) connection. The implants were 4.3 mm in diameter and 13 mm in length. The IH abutments were Universal Abutment II Plus (Neodent Implante Osseointegrável), a two-piece abutment with a fixation screw (Figs 1a and 1b).
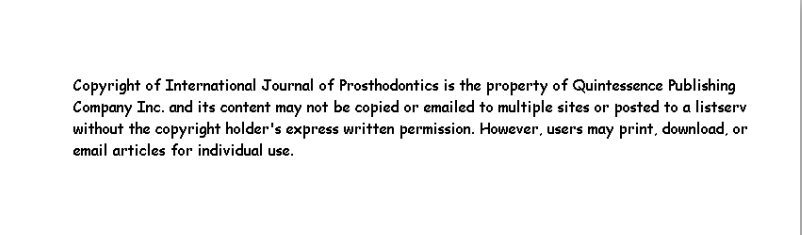
The IC abutments were Universal Abutment CM (Neodent Implante Osseo-integrável), a one-piece solid abutment with an apical threaded portion (Fig 1c). Ten implant-abutment assemblies were used for each system (Figs 2a and 2b). Installation torques were 10 Ncm for the IH abutments and 20 Ncm for the IC abutments, according to manu-facturer’s instructions, as measured by a digital torque meter (TQ680, Instrutherm). Different preload values were due to the different types of threads in each sys-tem (ISO M1.60 mm for the IH system and ISO M1.80 mm for the IC system).
a- Graduate Student, Department of Dental Materials and Prosthodontics, Dental School of Ribeirão, University of São Paulo, Ribeirão Preto, SP, Brazil. b- Professor, Department of Dental Materials and Prosthodontics, Dental School of Ribeirão, University of São Paulo, Ribeirão Preto, SP, Brazil. c- Assistant Professor, Department of Dental Materials and Prosthodontics, Dental School of Ribeirão, University of São Paulo, Ribeirão Preto, SP, Brazil. d- Assistant Professor, Latin-American Dental Research Institute (ILAPEO), Curitiba, PR, Brazil. Correspondence to: Prof Dr Ricardo Faria Ribeiro, Department of Dental Materials and Prosthodontics, Dental School of Ribeirão Preto, University of São Paulo, Av. do Café, sn- Monte Alegre 14040-904, Ribeirão Preto, SP, Brazil. Fax: +55 16 3602 0547. Email: rribeiro@forp.usp.br
The implants were embedded in a 21.3-mm- diameter by 25.6-mm-high stainless steel cylinder. The embedded depth was 10 mm to simulate a 3-mm bone resorption.4 Oblique compressive loading tests were made in a universal testing machine (DL-2000, EMIC). Loading was performed with the specimens positioned at a 45-degree angle, utilizing a 500 kgf load cell with 1 mm/min dislocation (Fig 2c). The loading point was at a distance of 11 mm from the cylinder surface (lever arm length).
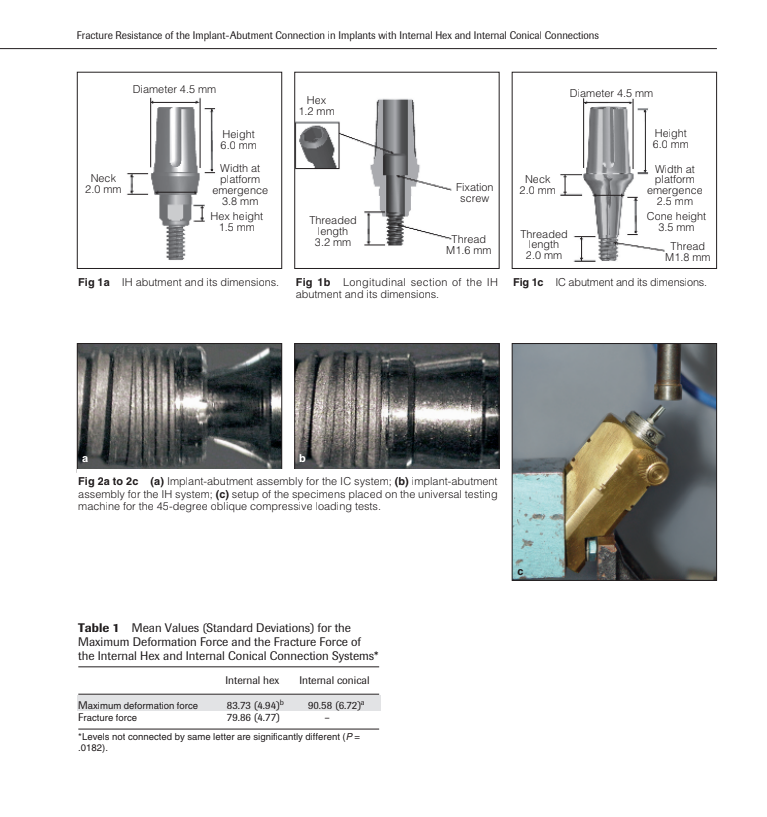
Two values were analyzed in each test: the maximum deformation force (MDF) and the fracture force (FF) of each implant-abutment assembly under 45-degree compressive loading. All results were ana-lyzed using statistical software (JMP for Windows ver-sion 5.1, SAS Institute). MDF values were assessed using the Student t test (P < .05).
Results
The MDF and FF values for each implant-abutment as-sembly were recorded and mean values and standard deviations are shown in Table 1. For all specimens, MDF occurred during the plastic deformation phase; after MDF was surpassed, either component frac-tures occurred (IH system) or a considerable decrease of the resistance force caused by continued implant-component deformation occurred (IC system). The highest MDF values were obtained by the IC system (90.58 ± 6.72 kgf) followed by the IH system (83.73 ± 4.94 kgf) (Fig 3). The Student t test revealed a signif-icant difference (P = .0182) between the two systems.
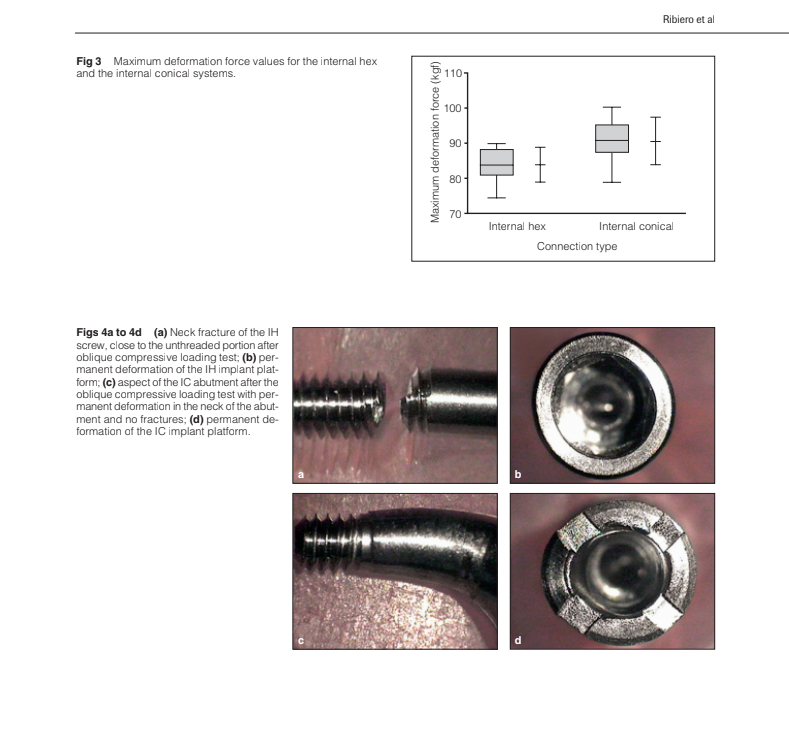
Only the IH assemblies fractured and had their FF recorded (79.86 ± 4.77 kgf). Optical micrographs showed that the fractures on the IH abutments always occurred in the fixation screws and permanent de-formations occurred in the implant platforms. The IC abutments showed permanent deformations in the neck. There were also permanent deformations in the implant platforms of the IC abutments; no fractures were detected in the abutments or implants (Figs 4a to 4d).
Discussion
All IH implants used in this study showed fractures in the fixation screw, while the IC implants showed no fractures. Both systems employed different mechani-cal principles of function. 5 In the IH configuration, the axial preload of the abutment screw was a primary fac-tor for stability of the connection and the screw alone secured the abutment. There was no form lock or pos-itive locking by the internal hex, which did not absorb any lateral loading. 5 Therefore, when oblique forces were applied to the implant-abutment assemblies dur-ing the tests, the yield point of the assemblies was ba-sically the yield point of the screws. In IC connections, form lock and friction were the primary principles.
Lateral loading was mainly resisted by the tapered in-terface, which prevented fractures of the abutments. Normal chewing forces have been reported in the lit-erature, ranging between 30 and 50 kgf in posterior re-gions. For all specimens tested, plastic deformations started to occur under oblique compressive loads of over 80 kgf. Thus, both systems presented an adequate resistance, which indicates that under normal occlusal conditions, both would present a successful clinical performance. MDF can be used as a parameter value of the oblique load each system is capable of resisting before destructive events occur.
Although MDF values were statistically different between the systems, these dif-ferences were not high enough to be considered clin-ically significant. If these systems were subjected to ex-cessive oblique compressive forces surpassing their MDFs, screw fractures would probably occur in the IH abutments, while permanent deformations would bemore likely to happen on the neck of the IC abutments. Either way, both systems would possibly show perma-nent deformations on the implant platform, resulting in failure of the treatment. These findings reinforce the importance of careful planning and refined occlusal adjustments, avoiding excessive oblique loads. Further studies are necessary to compare the fatigue resistance of both systems under dynamic cyclic loading in order to provide more accurate data concerning their long-term fracture resistance.
Conclusion
Under the conditions of this in vitro investigation, the results indicate that the friction-locking mechanics and solid design of the one-piece abutments of the IC connection system provided greater deformation and fracture resistance to the implant-abutment assembly under oblique compressive loading when compared to the IH connection system. Further in vitro and clinical investigations are needed to evaluate the fatigue re-sistance of these systems under long-term dynamic cyclic loading.
Acknowledgment
The authors would like to acknowledge Neodent Implante Osteo-integrável (Curitiba, Brazil) for providing the implant components.
References
- Maeda Y, Satoh T, Sogo M. In vitro differences of stress concen-trations for internal and external hex implant-abutment connec-tions: A short communication. J Oral Rehabil 2006;33:75–78.
- Bozkaya D, Müftü S. Mechanics of the taper integrated screwed-in (TIS) abutments used in dental implants. J Biomech 2005;38:87–97.
- Norton MR. An in vitro evaluation of the strength of a 1-piece and 2-piece conical abutment joint in implant design. Clin Oral Implants Res 2000;11:458–464.
- Khraisat A, Stegaroiu R, Nomura S, Miyakawa O. Fatigue resis-tance of two implant/abutment joint designs. J Prosthet Dent2002;88:604–610.
- Merz BR, Hunenbart S, Belser UC. Mechanics of the implant-abut-ment connection: An 8-degree taper compared to a butt joint con-nection. Int J Oral Maxillofac Implants 2000;15:519–526.